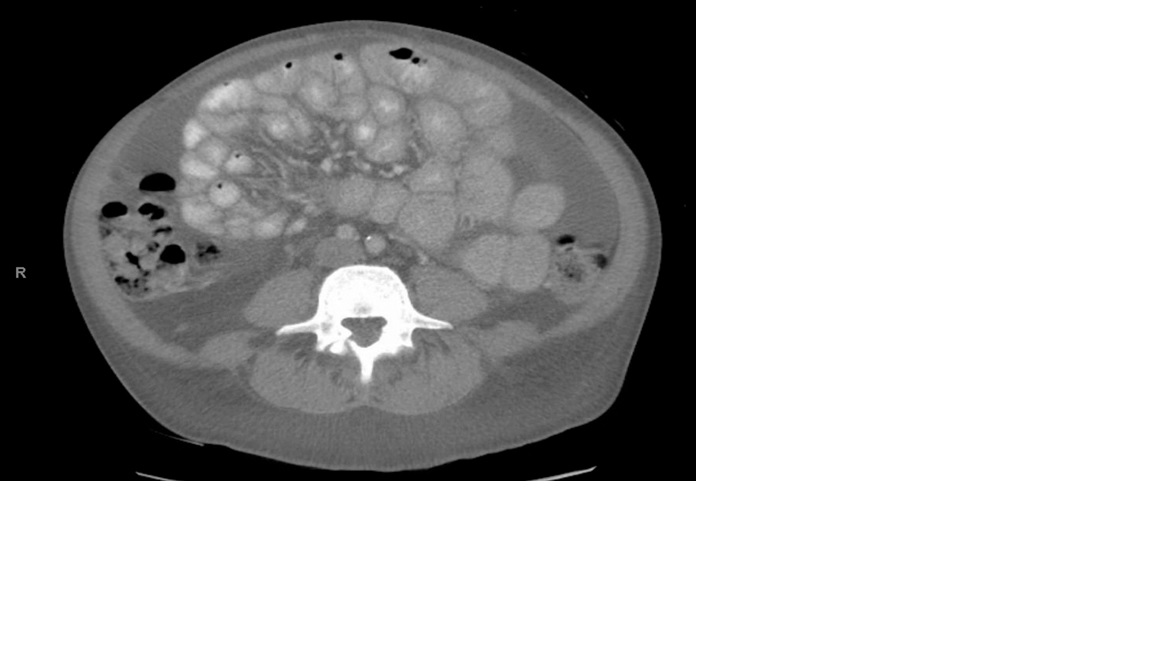
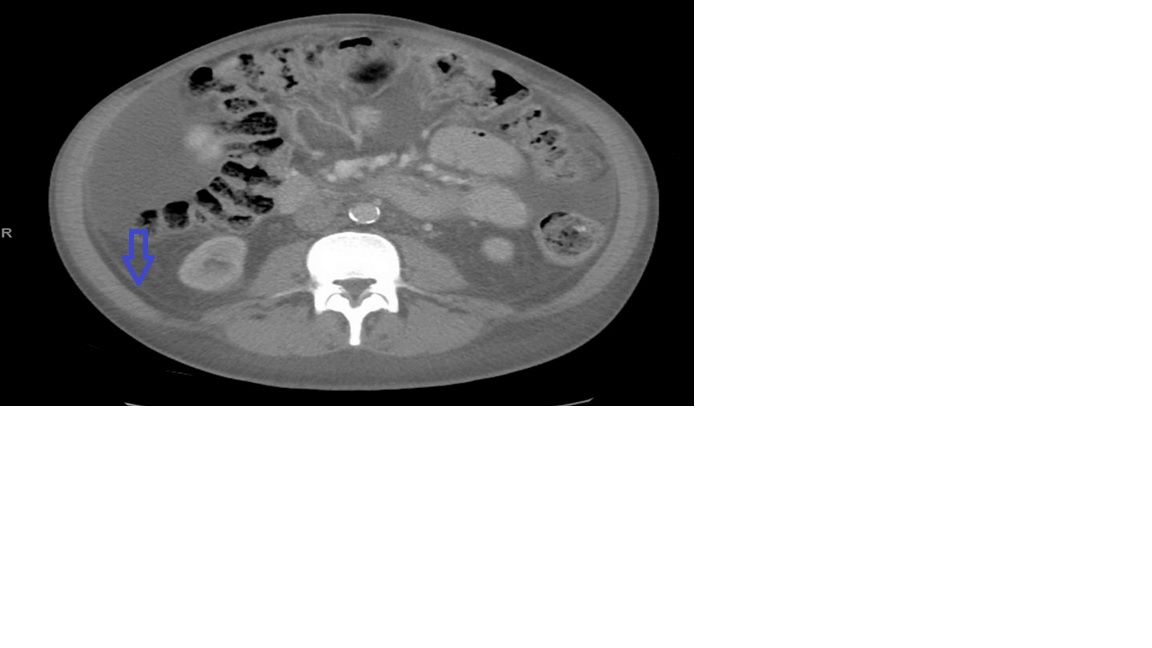
Case Presentation: 36-year-old male with past medical history of end stage renal disease (ESRD) on PD for 5 years, was admitted with chief complaints of abdominal pain, vomiting and diarrhea for 3 days. Examination revealed diffuse abdominal tenderness, without any rebound tenderness or guarding. PD catheter site was in place with no surrounding tenderness, or erythema. Laboratory markers revealed blood glucose of 593, metabolic acidosis with high anion gap, and WBCs of 12.4. CT abdomen without contrast showed small amount of ascites, otherwise unremarkable. Patients was managed with insulin drip and fluid therapy under the impression of diabetic ketoacidosis. Two days later, purulent discharge was noticed from the catheter site. Accordingly, empiric intraperitoneal antibiotics therapy was started. Peritoneal fluid analysis was performed, which showed WBC less than 5. However, antibiotics were discontinued and the PD catheter was removed due to concern of infection. HD was initiated through a temporary catheter. In a few days, his pain improved and he was discharged in good condition. Following discharge, he had 3 episodes of re-admission with similar complaints. CT scans were repeated for 3 times which showed ascites and minimal small bowel inflammatory changes. On further reviewing the CT scans, subtle peritoneal thickening was observed. The bowel loops were fixed in the same position on multiple CT scans over four months, which was consistent with loculation, a key feature of Encapsulating Peritoneal Sclerosis.
Discussion: Encapsulating peritoneal sclerosis (EPS) is an uncommon, but devastating complication after long-term peritoneal dialysis (PD). EPS is characterized by slowly progressive peritoneal fibrosis, leading to encasement of the bowel, which may result in bowel obstruction and ultrafiltration failure.In order to diagnose EPS, specific EPS scoring system can be used. Treatment of EPS includes tamoxifen, sirolimus, steroids and/or enterolysis.
Conclusions: EPS incurs high morbidity and mortality. The clinical findings of EPS can be vague, with subtle radiologic findings. This case highlights the importance of suspecting EPS as a potential cause of recurrent ascites and abdominal pain in a patient on chronic PD.Our patient was initiated on tamoxifen and tapering course of steroids on discharge.