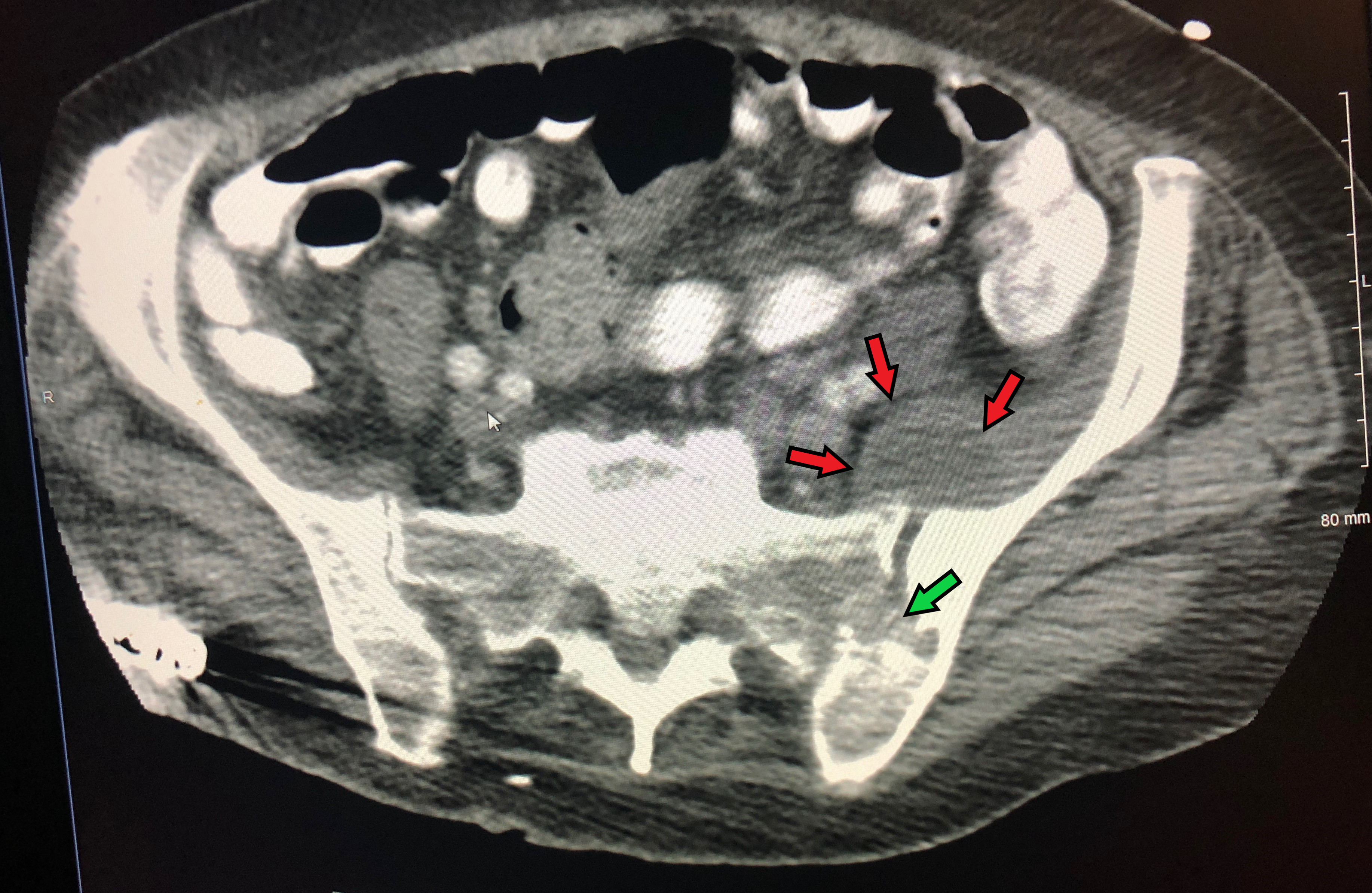
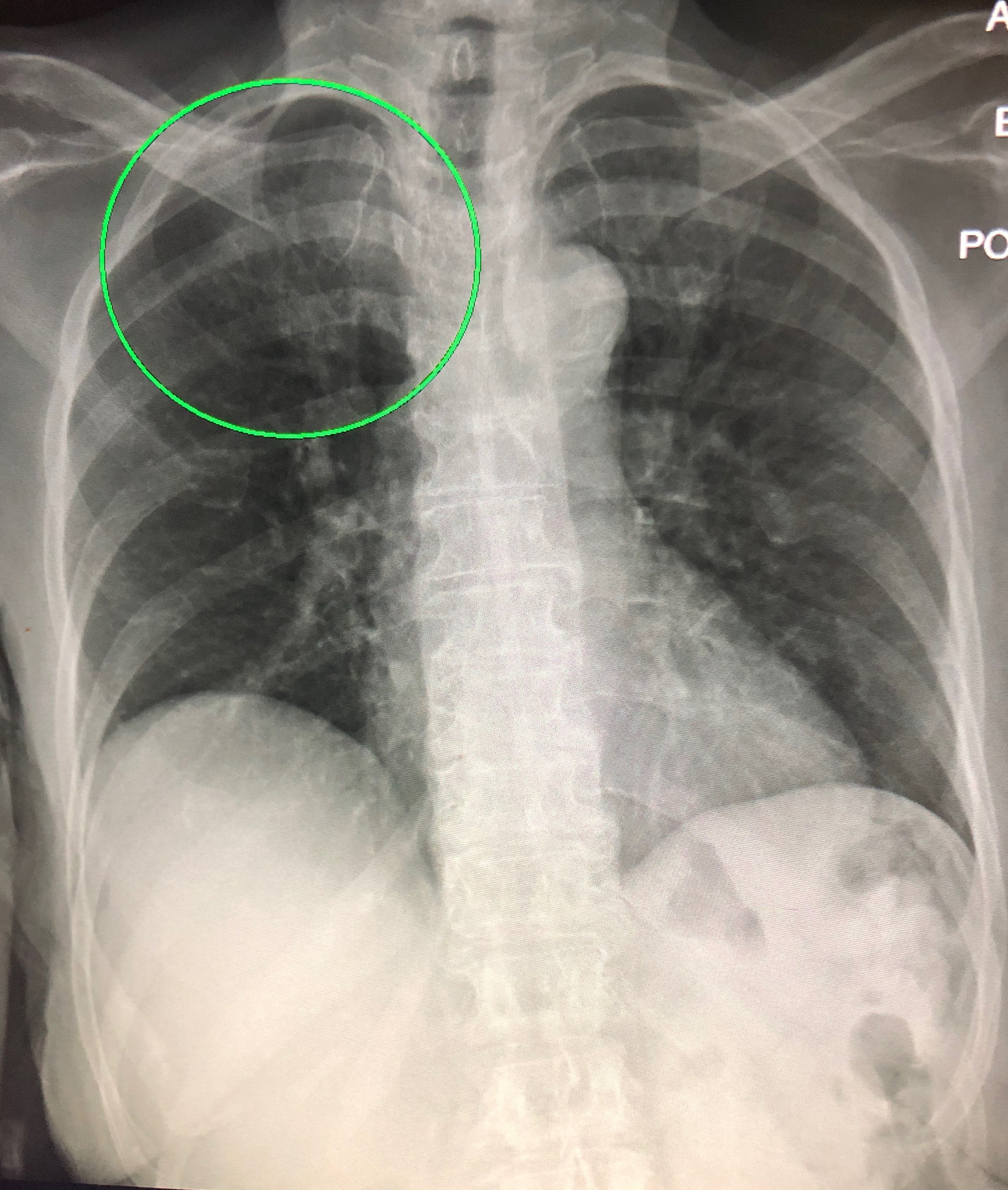
Case Presentation: A 77-year-old African American female with rheumatoid arthritis on chronic prednisolone presented with fever, weakness and unsteady gait. Further history revealed latent tuberculosis (TB) infection treated over 15 years ago and granulomatous abdominal lymphadenopathy three years ago. Physical exam revealed fever and limited left hip mobility due to weakness and pain. Labs showed leukocytosis of 35,000 and computed tomography (CT) of the hip joint revealed destruction of left sacroiliac joint, osteomyelitis and an abscess near the left iliopsoas muscle (Figure 1). She was started on broad spectrum antibiotics for pyogenic sacroiliitis, osteomyelitis and left psoas abscess and underwent partial excision of her sacroiliac bone and drainage of neighboring abscess. Gram stain, Acid fast bacillus (AFB) stain and bacterial culture of the abscess were negative and bone pathology revealed ill-defined granuloma. Samples were sent for tuberculosis culture. One of four blood cultures grew Enterococcus faecalis. Given that all other testing was negative, the patient was sent home with intra venous ampicillin with sensitivity for six weeks through a peripherally inserted central catheter. Two days after antibiotic completion the patient presented to the hospital with night sweats and weakness. Chest x-ray revealed right upper lobe pulmonary infiltrates (Figure 2) and coincidentally, the previous AFB culture came back positive that same week and TB was confirmed by polymerase chain reaction (PCR) from the culture positive specimen. Isolation precautions and rifampin, isoniazid, pyrazinamide and ethambutol (RIPE) therapy were started. After two weeks, she had marked improvement along with negative AFB-PCR smear in her sputum. Isolation precautions were discontinued, and she was discharged with instructions to follow up with public health department.
Discussion: TB is a leading cause of death worldwide and musculoskeletal TB is reported in 3-5% of cases.[1] We report a case of musculoskeletal TB initially misdiagnosed as enterococcus sacroiliitis. Negative culture and stains and enterococcus bacteremia appropriately dictated immediate antibiotic therapy but caused anchoring to a diagnosis without considering the patient’s high risk for concomitant TB. In the case of a patient with known TB exposure and chronic immunosuppression, granulomatous bone biopsy and biopsy proven granulomatous nodules should have led to earlier PCR testing or empiric TB treatment at presentation.[2] We believe radical debridement and drainage and partial activity of ampicillin against TB might have kept the disease under control for the 6-week treatment.
Conclusions: Tuberculous sacroiliitis is a disabling condition and can often be overlooked.[3] A high index of suspicion and rapid detection with TB-PCR testing should be considered to avoid delayed diagnosis and increased morbidity.