Background: Communication is a vital aspect of a doctor-patient relationship in providing medical care. Despite extensive research and ACGME guidelines of interpersonal and communication skills, there is a lack of a formal curriculum that is designed to systematically teach resident physicians on creating and sustaining therapeutic relationships with patients and families. Some institutions have tried to implement a long term communication curriculum, which include monthly conferences, simulated clinical experiences, and regular faculty feedback, and addresses multiple different components of communication over an entire training period. These long-term curricula have yielded positive results in self-reflections when comparing doctor-patient communication skills at the beginning of intern year to graduation.
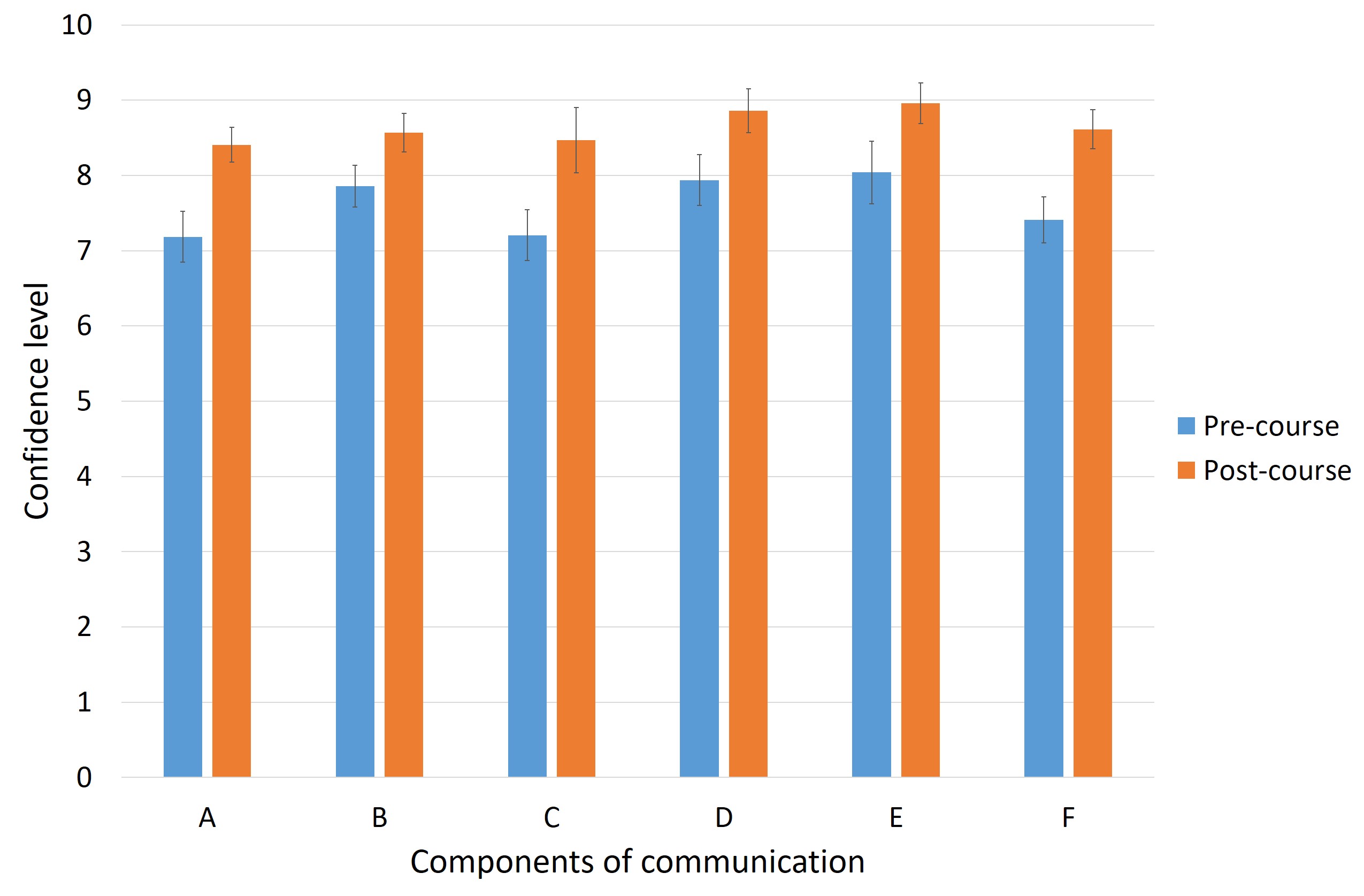
Methods: Our institution provided a one-time two hour session addressing relationship centered communication skills for residents in training. Self-reflection surveys were conducted before and after the training session to evaluate the impact of the course on confidence levels in six different disciplines of communication (A: Overall communication skills ability, B: Creating rapport with patients, C: Elicit patient concerns, D: Demonstrate active listening, E: Ability to respond with empathy, F: Communicating the information to the patient).
Results: Pre and post surveys showed that resident confidence levels increased among all six components of communication across all PGY years. Despite the overall increase in confidence there was a widespread difference in the change in confidence among the different years. PGY2s had the most change in confidence with respect to communicating to patients and eliciting their concerns whereas PGY3s had the most change in confidence with respect to creating rapport with patients. The surveys indicated that our residents enjoyed role-playing scenarios more than lecture-style teaching during this training course and would prefer more interactive sessions to build their communication skills.
Conclusions: It is clear that a formal communication course outlining different components of communication is beneficial for resident physicians during their medical training. It would be most effective to start this course at the beginning of residency and to monitor longitudinal growth until graduation with periodic faculty feedback and interactive sessions to practice these new skills. Our next steps aim to include more role-playing than lecture-style teaching and to capture the impact of the training via patient surveys rather than just resident confidence.