Background: Affecting approximately 5.9% of the US population, alcohol use disorder (AUD) has been established as a prevalent disease in this country (1). Through repeated hospital admissions for alcohol use disorder (including alcohol withdrawal syndromes), hospital costs have steadily risen to recent estimates of 7.6 billion dollars in 2017 (2). Without the establishment of outpatient support and treatments for alcohol use disorder, these patients are at high risk for readmission and prolonged hospital stays, which can be frustrating to both the patients and healthcare providers. Furthermore, untreated AUD can lead to liver and other vital organ complications.
Purpose: Focusing on Greenwich Hospital, a small community-based hospital in Connecticut, we aimed to reduce length of stay, readmission rates, and use of unnecessary benzodiazepines through a multidisciplinary approach to the treatment of alcohol use disorder and alcohol withdrawal syndromes in hospital. In an effort to further address deficits in outpatient follow-up and treatment of AUD at discharge, we focused on increasing adherence to a standardized treatment pathway with a targeted goal of readmission rate reduction, as has been shown in previous studies (3 – 4).
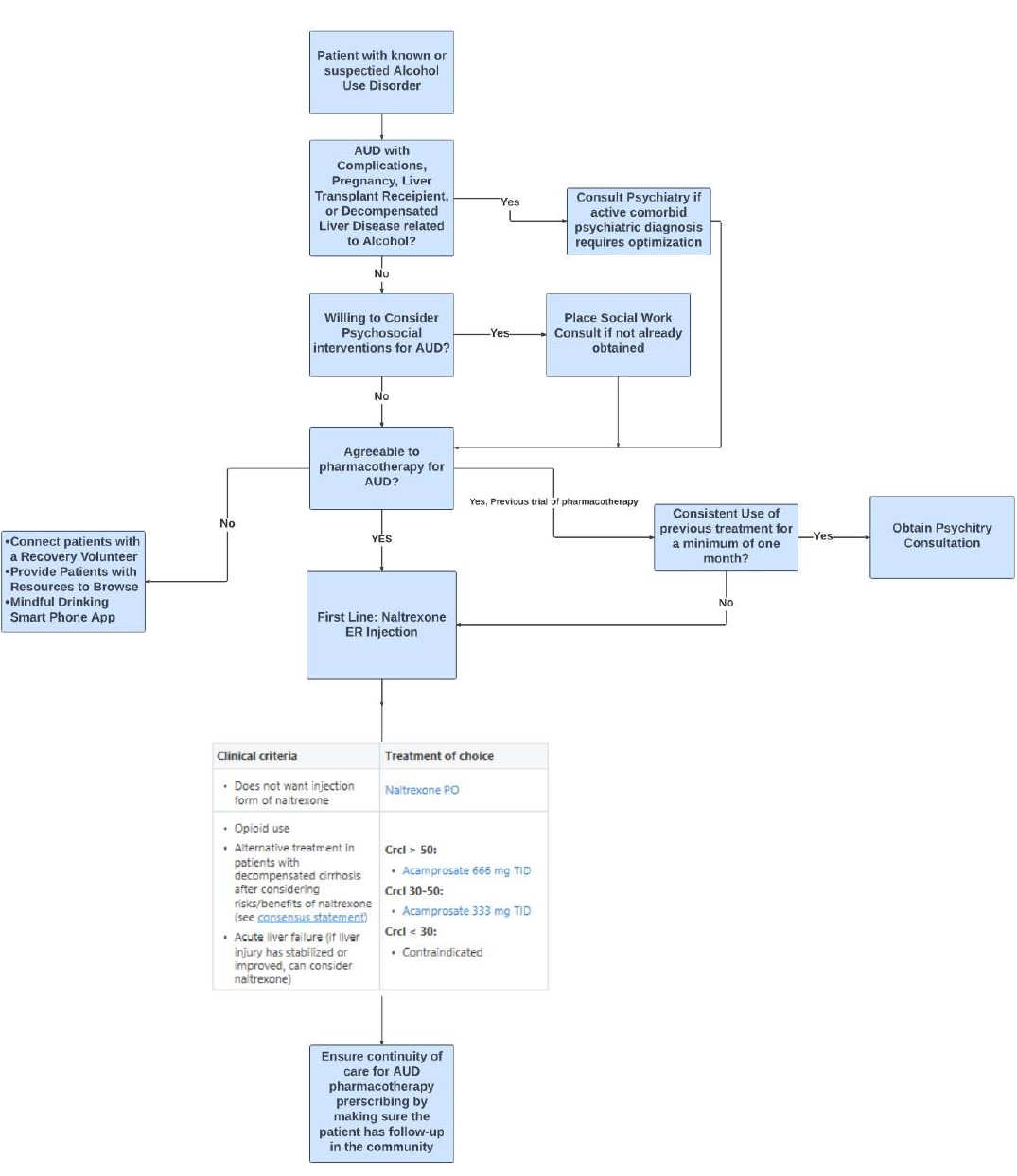
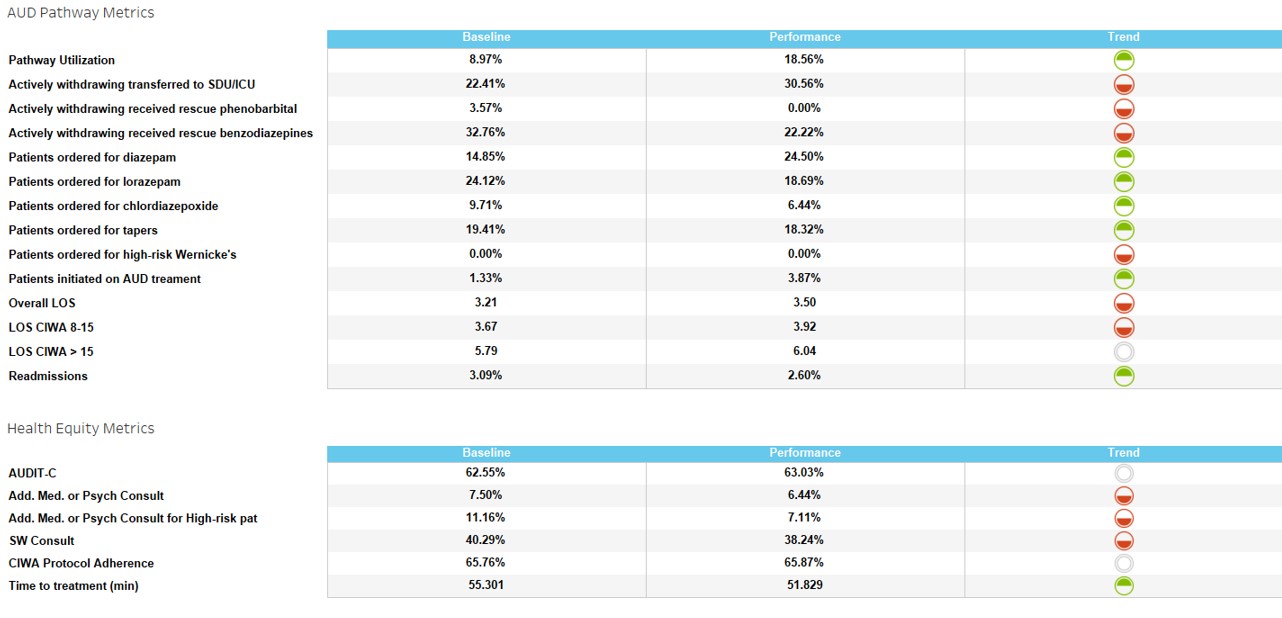
Description: Several metrics including length of stay (LOS), librium usage, readmission rates, and pathway utilization were observed in 12-month periods before and after efforts were made to improve systematic practices. The key drivers of change focused on the utilization of an AUD treatment pathway integrated into the electronic medical record, improving implementation of CIWA scoring by nursing, and reduction of alcohol withdrawal syndrome medications ordered outside of the pathway recommendations (such as Librium) by empowering pharmacy staff to question provider orders. To improve pathway utilization, we made the AUD pathway easier to access and focused on provider education. While these changes targeted the inpatient setting, we also worked on improving outpatient discharge planning, including prescribing AUD medications upon hospital discharge. This was outlined in our EMR care signature pathway as seen in Figure 1. Following a period of 12 months following practice improvements, the changes observed at Greenwich Hospital are noted in Table 1. Compliance towards pathway utilization increased by 100%. Librium usage decreased by 33%, AUD treatment initiation increased by nearly 300%, and readmission rate decreased by 16%. However, overall length of stay remained relatively unchanged, indicating that our systematic changes may have better served readmission rates and outpatient treatment of AUD.
Conclusions: Through increased adherence to a standardized protocol for alcohol use disorder, we have demonstrated a marked improvement in the treatment of AUD to prevent further readmissions correlating with an increased inpatient treatment with craving-reducing medications at discharge. Outpatient treatment of AUD still has room for further optimization. Utilizing previously identified predictors of relapse including younger age, presence of psychiatric illness, and prolonged treatment episodes, we may be able to treat vulnerable patients better and further decrease their readmission rates (5). With only 18.65% of our patient encounters for AUD utilizing the pathway, there is still opportunity for further provider education, which may help in reducing length of stay.