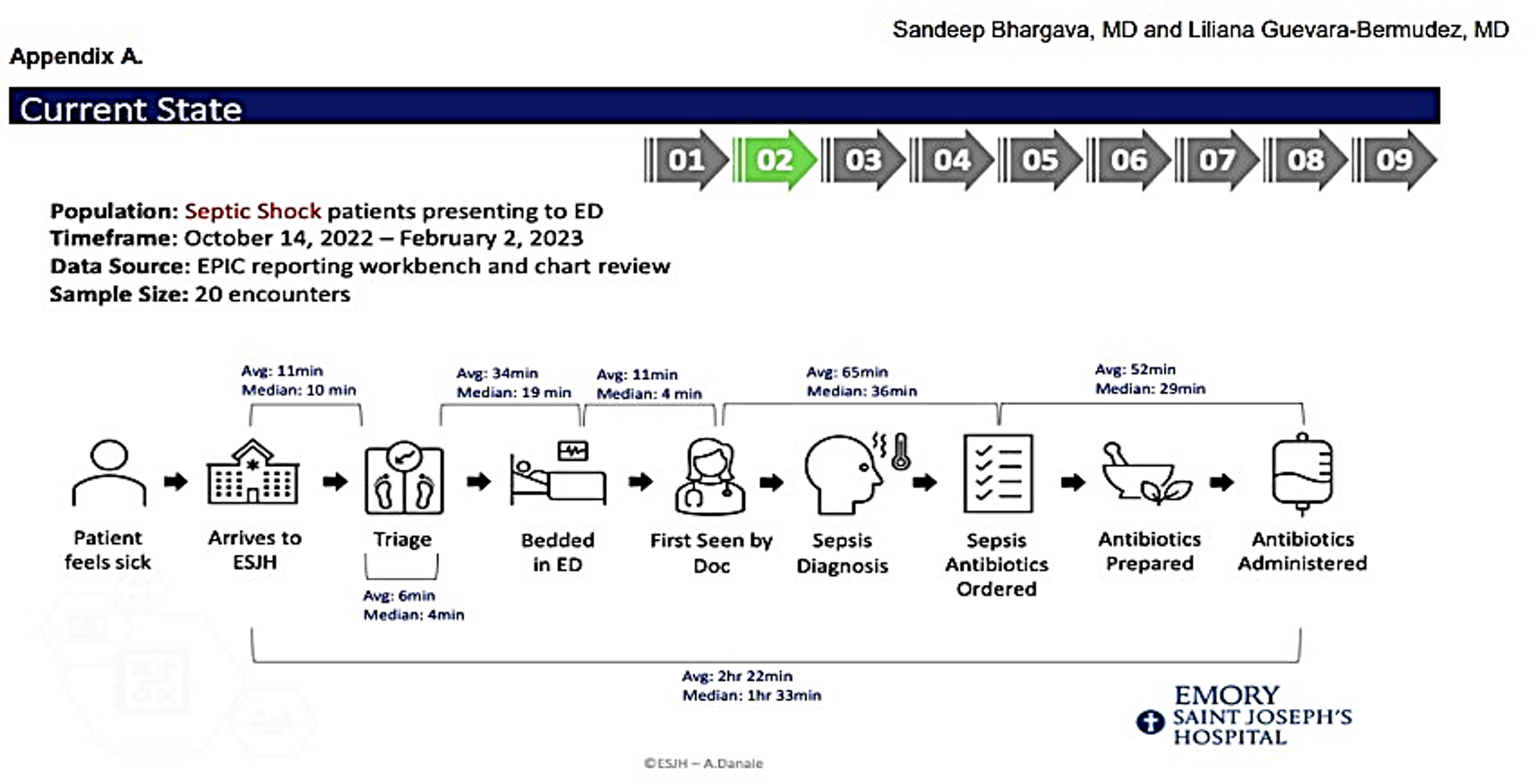
Background: Septic shock is a significant burden: average length of stay (LOS) for sepsis patients in US hospitals is 75% greater than most other conditions. Mean LOS dramatically increases with sepsis severity: 4.5 days for sepsis, 6.5 for severe sepsis, and 16.5 for septic shock. Administration of antibiotics in < 1 hour after presentation at a hospital improves patients' survival and LOS but requires prompt recognition of septic shock and efficient processes. The current average time from ED presentation to administration of antibiotics at our institution is 2 hours 22 minutes, significantly greater than that indicated by the for Medicare & Medicaid Services’ (CMS) SEP-1 guidelines. We have collected data on existing processes to prepare and implement a quality improvement initiative to reduce time between initial emergency department (ED) presentation of patients in septic shock to early administration of antibiotics at Emory Saint Joseph’s Hospital (ESJH) from its current average state, >2 hours, to < 1 to comply with CMS' SEP-1 guidelines. In this abstract, we present preliminary data and describe our proposed interventions to understand and reduce the time interval from admission to antibiotic administration.
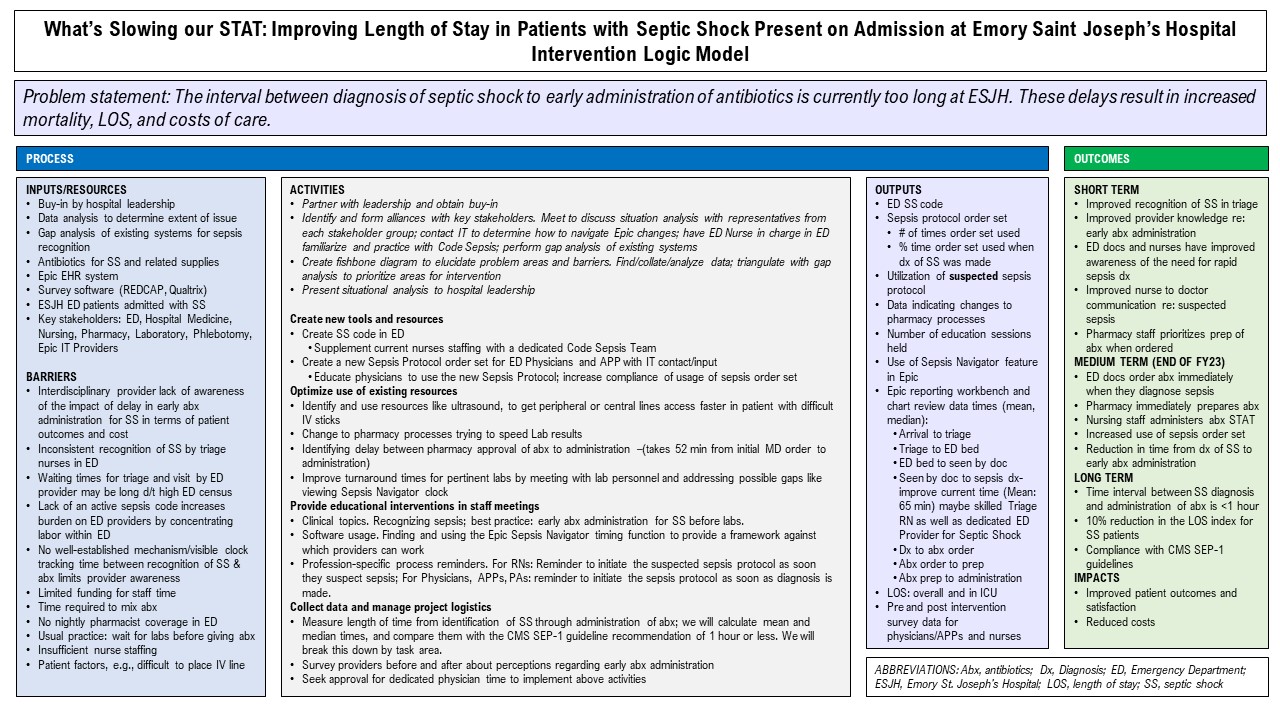
Methods: To understand our institutional context, we first partnered with leadership to obtain buy-in. We identified and formed alliances with key stakeholders, performed a gap analysis of existing systems, and created a fishbone diagram to elucidate problem areas and barriers.We will collect data and measure change with descriptive statistics. We will continue to measure average and median time from identification of septic shock through administration of antibiotics and assess provider perceptions regarding early antibiotics administration for septic shock via survey. We will then triangulate these data with our gap analysis to prioritize areas for intervention (see Logic Model diagram for an overview of our planned intervention).
Results: We looked at FY 2022 patients with septic shock present on admission and saw that patients who had excess LOS days contributed to excess care costs of $1.3 million. We found that within the >2-hour time from ED presentation to administration of antibiotics, the longest intervals were between when a patient is first seen by a provider and STAT antibiotics are ordered (mean 65 minutes, median 36 minutes) and between when antibiotics are ordered and administered (mean 52 minutes, median 29 minutes) (Figure 1).
Conclusions: We aim to improve recognition/diagnosis of septic shock in triage, increase ED provider awareness of/communication around need for rapid sepsis diagnosis, and facilitate pharmacy staff prioritization of STAT antibiotics orders. The greater mean times than median times in intervals between steps raises concern that outliers are making excess contributions to delays; we intend to investigate and determine if these can be remediated. Moving forward, we will implement targeted interventions raising awareness through educational activities; identifying and remedying process inefficiencies; modifying the ED sepsis order set to incorporate STAT antibiotics; building staff capacity to identify septic shock and use protocols; establishing a sepsis code team in the ED; and utilizing existing technology (e.g., Epic Sepsis Navigator).Long-term, we aim to decrease time from diagnosis to antibiotic administration to < 1 hour, in compliance with CMS SEP-1 guidelines, eventually improving patient outcomes and satisfaction and reducing costs.