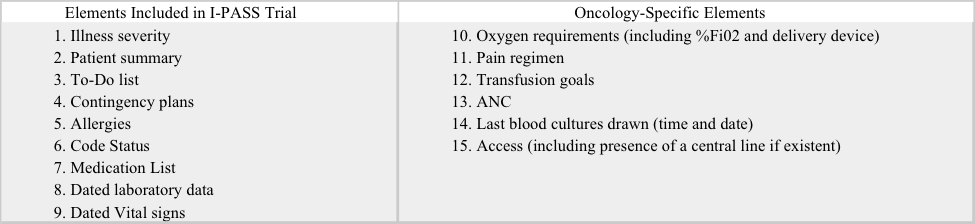
Background: Standardizing inter-shift handoff procedures enhances continuity of care and quality with an associated reduction in preventable medical errors. This is particularly relevant in the inpatient oncology population where patients have a relatively high morbidity/mortality compared to the general inpatient population. With increasing handoffs due to work hour restrictions, and rising utilization of multidisciplinary teams, it is important to optimize handoff. We identified several oncology-specific key elements for inclusion in a standardized handoff tool (table 1) that, in conjunction with educational efforts, lead to a significant improvement in our handoff procedures.
Methods: Our study consisted of: 1) An artifact analysis of handoff documents and 2) Surveys and interviews of clinicians. We created a customized, EHR-based handoff tool and conducted educational presentations of the new handoff functions, emphasizing key data inclusion. We surveyed clinicians before and after the intervention and assessed satisfaction and perceived time spent on handoff. We examined pre and post intervention handoffs to measure inclusion of 15 key elements. We compared rates of inclusion for each element using fisher’s test. In addition, we analyzed the percentage of key elements included overall pre and post intervention using a Wilcox Rank Sum Test.
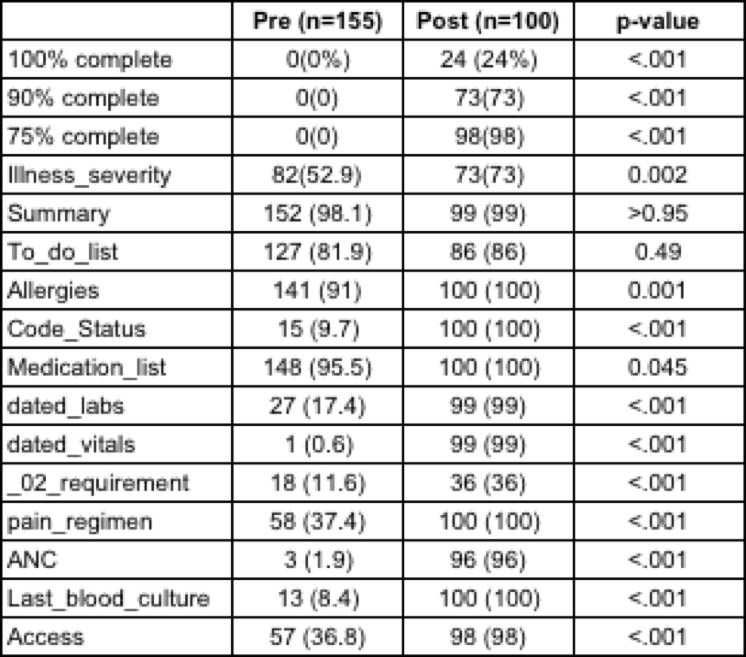
Results: 155 pre-intervention and 100 post-intervention charts were assessed from 5 services (leukemia, lymphoma, bone marrow transplant, thoracic and sarcoma). The percentage of handoffs with labs (post 99% vs. pre 17.4%; p<0.001), an accurate pain regimen (100% vs. 37.4%; p<0.001) and type of IV access (98% vs. 57%; p<0.001) increased by a large proportion. Other elements had modest but statistically significant increases, such as oxygen requirements (36% vs. 11.6%, P<0.001) and illness severity index (73% vs. 52.9% p<0.002). Inclusion rates for two elements, the presence of a summary (99% vs. 98.1%; p>0.95) and to-do list (86% vs. 81.9%; p=0.49) did not increase substantially.
24% of our post-intervention charts included every element, an increase from 0% pre-intervention (p<0.001). 100% of our pre-intervention handoffs were missing at least 25% of the data elements, this dropped to 2% post-intervention (p<0.001). Prior to the intervention, 34.2% (13/37) of clinicians surveyed spent >10 minutes updating the handoff daily. This decreased to 17.6% (3/17) after the intervention. 43.2% (16/37) of clinicians surveyed were able to update the handoff in 6 minutes or less prior to our intervention, this number increased to 64.7% (11/17) after the new handoff tool was implemented.
Table 2 includes the complete results of our artifact analysis.
Conclusions: Implementation of a standardized tool resulted in a significant increase in quality and reliability. Identifying data elements critical to a certain population allows for a tailored approach to the handoff process. Our intervention significantly increased the inclusion of key oncology-specific data elements. This was associated with a perceived decrease in the time spent on handoff and an increase in clinician satisfaction.