Background: As of 2020, a reported 2.7 million people in the United States have opioid use disorder (OUD). Hospitalizations related to opioid use have risen dramatically over the last two decades. Inpatients with substance use disorders are at increased risk of leaving the hospital prior to treatment completion which can further lead to poor health outcomes. We sought to determine the association between inpatient treatment with medication for opioid use disorder (MOUD) and patient directed discharge (i.e. discharge against medical advice).
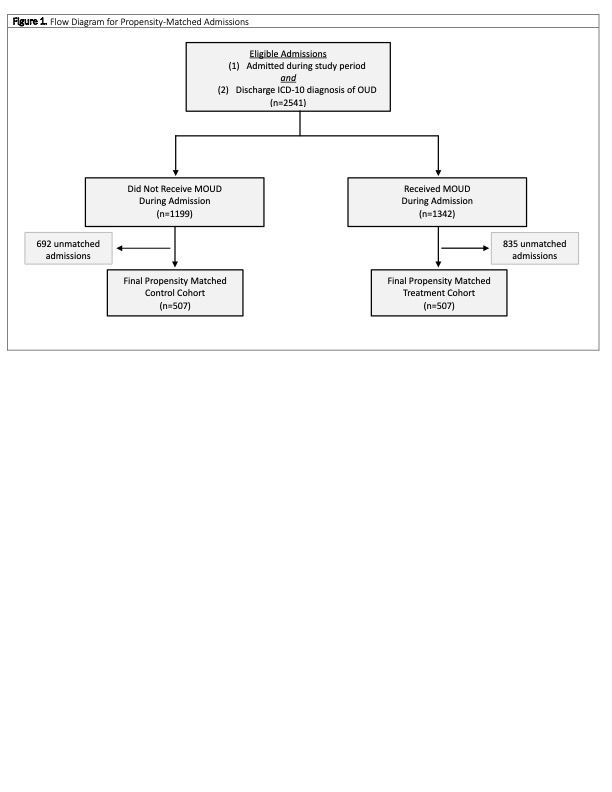
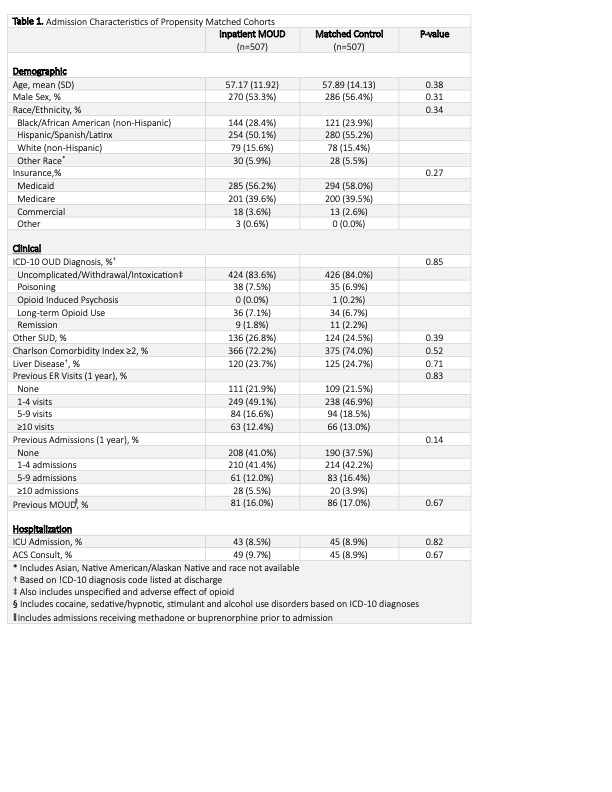
Methods: We used a retrospective propensity-score matched design to evaluate the impact of inpatient MOUD on admissions with an opioid related diagnosis. Inpatient MOUD was defined as treatment with methadone or buprenorphine, medications which are the most used FDA approved medications for the treatment of OUD and exhibit the most evidence of benefit in the outpatient setting. Each admission with an opioid related diagnosis who received MOUD was propensity-score matched with a control admission which did not receive medication. The propensity score was determined using a non-parsimonious 29-variable model including demographic, clinical, and admission-level covariates. The primary outcome was patient-directed discharge. Secondary outcomes included buprenorphine prescription at discharge, 30-day readmission, and 30-day post-discharge ER visit. Unadjusted and adjusted associations between MOUD and each of the outcomes were determined using univariable and multivariable logistic regression. Subgroups which might exhibit the greatest benefit from treatment were determined a priori and analyzed using univariable and multivariable logistic regression.
Results: Among admissions with an opioid related diagnosis, there were 507 admissions which received MOUD while admitted matched with 507 control admissions yielding a study sample of 1014 admissions. Admissions receiving MOUD had a significantly reduced likelihood of a patient-directed discharge compared with control admissions (8.9% vs 14.6%, OR 0.57 [CI 0.38-0.86]). Admissions receiving inpatient MOUD were also more likely to be discharged with a prescription for buprenorphine when compared with control admission (6.5% vs 1.4%, OR 4.97 [CI 2.23-11.09]). Inpatient MOUD was not associated with a reduction in 30-day readmission or post-discharge ER visit.
Conclusions: Inpatient MOUD was associated with a significant reduction in patient-directed discharge in this patient population which is at high-risk for increased mortality and morbidity. Treating patients with MOUD can increase their likelihood of remaining hospitalized to complete treatment for their presenting condition. These finding suggest meaningful benefit to treatment with MOUD among those with OUD.