Background: A key factor contributing to physician burnout is what is known as “pajama time”—the time spent on clinical tasks outside of regular working hours. For inpatient physicians, responding to after hours texting may contribute significantly to pajama time.
Purpose: At our large, urban academic medical center, 163 medicine residents rotate through the general medicine inpatient service, adhering to scheduled duty hours and transitioning patient care responsibilities to the next provider at the end of their shifts. As part of a wellness initiative aimed at addressing burnout, we sought to assess the prevalence of “pajama time” among residents. Through an initial survey, we identified that after-hours communication via the EMR-based messaging platform, Epic Secure Chat (ESC), contributed significantly to pajama time. We developed a quality improvement (QI) project to decrease the number of off-duty ESC messages.
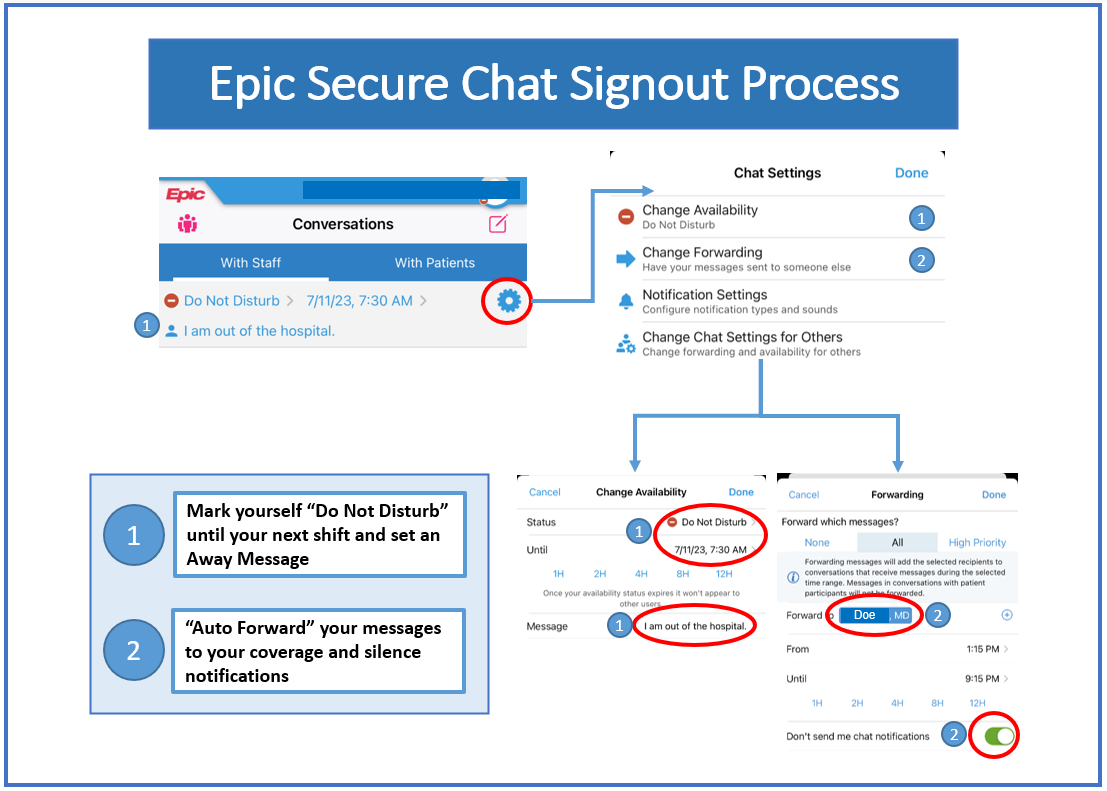
Description: We implemented a new workflow to sign out of the ESC system at the end of shifts. Residents were instructed to put away messages, forward messages to on-shift providers, and silence notifications. We tracked the number of off-duty ESC chats sent by categorical medicine residents on inpatient rotations from March 2023 through October 2023. From March to May, an average of 40 off-duty chats were sent per week, with a weekly range of 26 to 57 chats. However, after July 2023, the number of off-duty chats increased significantly, reaching an average of 104 chats per week, with a range of 32 to 190 chats.To understand the reasons behind this increase, we analyzed a random sample of 74 after-hours messages. We found that 47.3% of these conversations were initiated by non-physician healthcare professionals, while 52.7% were initiated by physicians. Among non-physicians, most messages came from pharmacists (29%) and nurses (23%). These messages were primarily directed to on-shift overnight residents (28%) and registered nurses (23%), with the off-duty resident often included. The majority of messages (46%) were related to EMR order requests, followed by patient status updates (16%) and handoff communications (16%). Notably, 64% of these conversations were deemed urgent, while 36% were considered non-urgent. In addition, we surveyed a small group of 11 residents regarding their adoption of the EMR signout workflow. Despite our interventions, only 4 residents used the availability status feature, and just 1 resident used the away message on ESC. Most residents reported responding to clinical questions sent to them via ESC during off-duty hours.
Conclusions: To reduce pajama time, we implemented a workflow enabling residents to forward messages, set away messages, and silence alerts on the secure messaging platform. However, we observed a decline in the use of this workflow after the start of the academic year, which coincided with an increase in messages sent by residents after their shifts ended. These findings highlight the challenges trainees face when adopting new workflows, particularly during the transition into the academic year. Additionally, our analysis revealed that many of the off-duty messages were initiated by nurses and pharmacists, who may not have recognized that the residents were no longer on duty. To address this, we are currently implementing a second PDSA cycle, which involves proactively reaching out to residents who send off-hour messages to reinforce the use of the suggested messaging workflows.