Background: Healthcare expenditures in the US have been increasing at an unsustainable rate, and thus there is a strong interest in resource stewardship of low-value diagnostic tests. At our institution, internal data, as well as The Vizient™ Clinical Data Base, showed high utilization of inpatient daily labs (complete blood count (CBC), basic metabolic panel (BMP) and complete metabolic panel (CMP)) across our multi-hospital healthcare system. We undertook a multidisciplinary approach to address laboratory utilization.
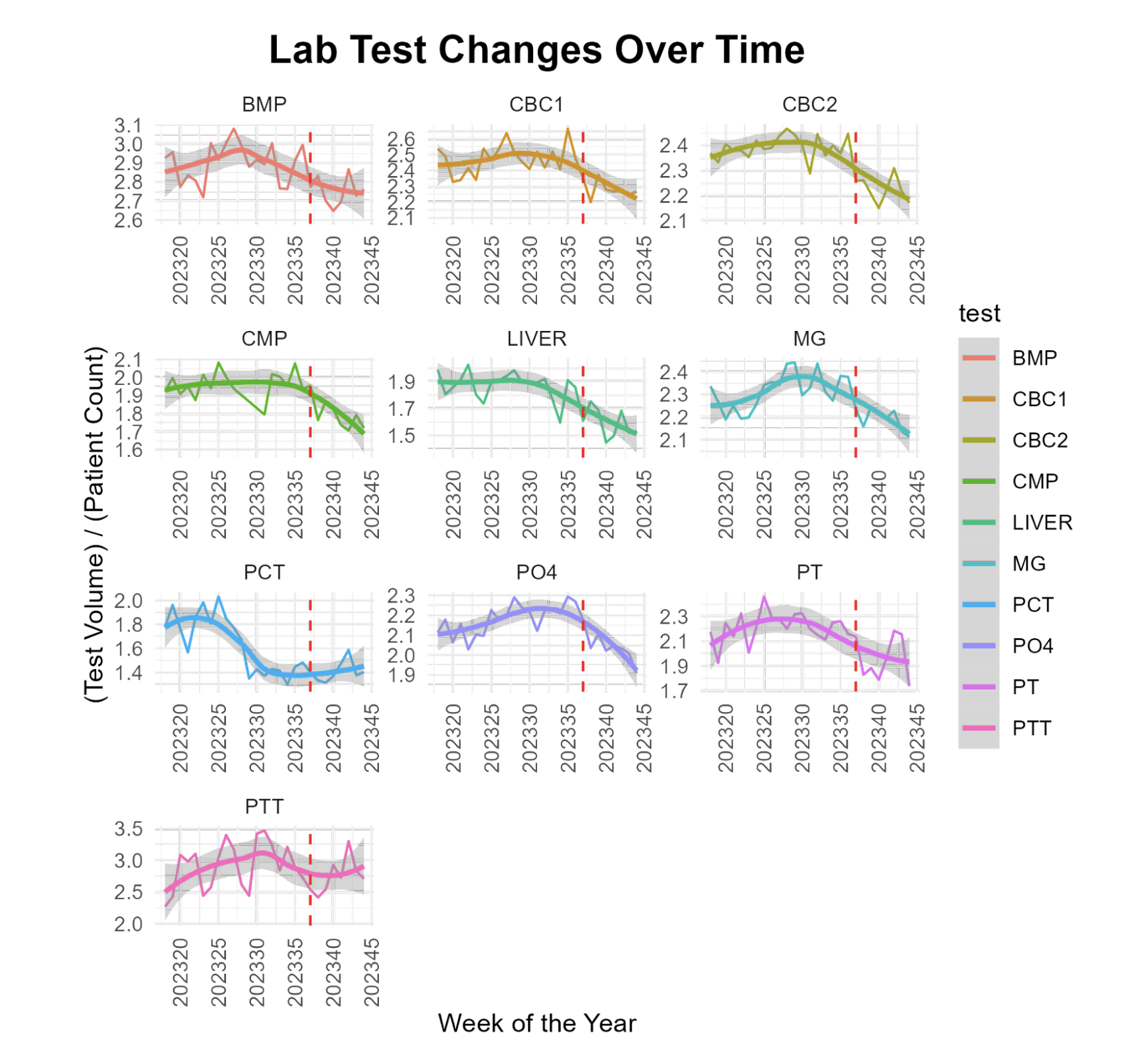
Methods: A multidisciplinary team, supported by our System Chief Clinical officer, designed an initiative to steward lab utilization. This included the Chief Medical Officer (CMO) and representatives from Information technology (IT), hospital medicine and laboratory services. As a group, we implemented an electronic medical record (EMR) change limiting standing orders for daily labs to a maximum of 3 days, after which they would need to be renewed if clinically indicated. Given our institution’s average length of stay (LOS) of about 4 days, a 3 day limit seemed appropriate. If ongoing labs were needed clinically, the physician could click a renew button to reorder the labs. The plan was widely discussed among inpatient services. The intensive care unit (ICU) expressed concern about missing key labs (INR, PTT and PT) leading to adverse impact (particularly on ECMO patients on heparin drip) so these were excluded from the intervention.Once we had frontline buy-in, we worked with IT to implement the system-wide change at 4 hospitals. Educational sessions and EMR changes were shared with rationale for the frontline teams, including our resident teams. Our intervention went live on September 12th, 2023. We looked at the total number of inpatient orders for BMP, CBC, Magnesium (Mg), Phosphate (PO4), CMP, PT, Liver Panel, PTT and Procalcitonin. We also looked at balancing measures of adverse events from no lab orders by monitoring through our event reporting system. Data was collected for 19 weeks prior to the change to establish baseline test volumes and 8 weeks after the change to measure the impact of the intervention.
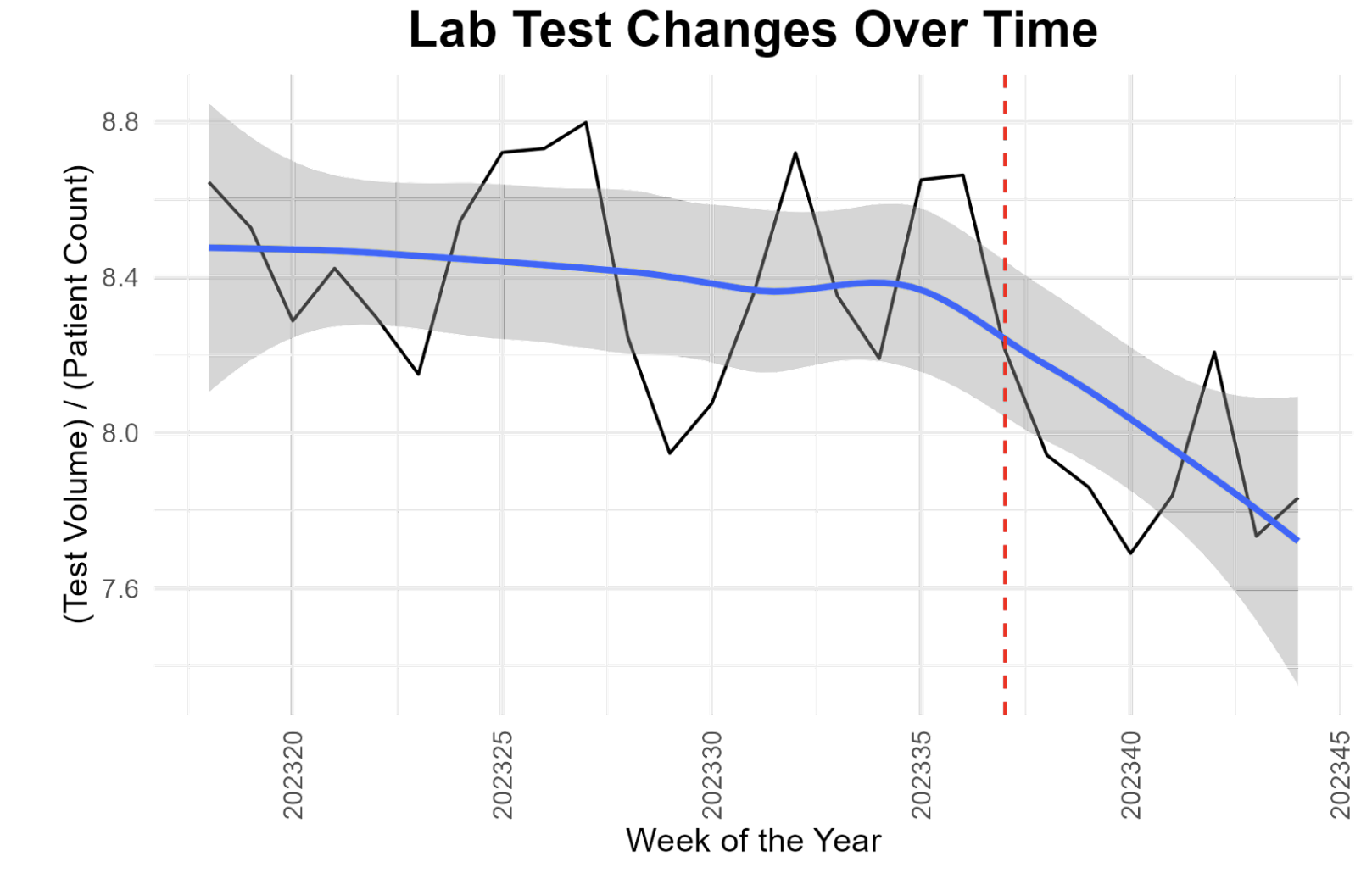
Results: Prior to our intervention, our internal lab data showed a median of 14,323 tests per week (interquartile range (IQR) = 637.5), with a median of 8.42 tests per patient per week (IQR = 0.4). After implementation of lab stewardship by limiting it to 3 day orders, we see the median drop to 13476 tests per week (IQR = 523), a reduction in 847 fewer tests per week with a p-value of < 0.01 (wilcoxon rank sum test). The median also dropped to 7.84 tests per patient per week (IQR = 0.1), resulting in 0.58 fewer tests per patient per week, with a p-value of < 0.01 (figure 1). We see downtrend trends in CBC,CMP, BMP, liver panel, magnesium and phosphorus. As expected, there was no change in PTT and PT (as they were excluded from the 3 day limit). There were no reports of adverse events or delay in care noted through our event reporting system.
Conclusions: Implementation of strategic EMR changes, combined with frontline buy-in, can significantly help with lab stewardship and without any reported adverse events. Long term data needs to be collected to see if this intervention remains effective. In the future, we plan on looking at financial cost savings, and other balancing measures such as “stat” lab ordering.