Case Presentation: An 11 year old boy was admitted to the hospital due to 4 days of headache and vomiting. He described the pain as constant, sharp, occipital/frontal in location, and worse in the morning and overnight, specifically with laying down. Treatment with ibuprofen and acetaminophen had not provided relief.
6 months prior to this admission he was hospitalized with fevers, skin bruising, epistaxis, fatigue, and spontaneous loss of an adult tooth. Laboratory studies at that time showed a mild eosinophilia, transaminitis, elevated CRP and creatinine. MRI of the brain looking for Langerhans cell histiocytosis was unremarkable. After discharge, extensive outpatient workup for other immunodeficiencies was unremarkable, but did reveal an elevated IgE level of 1,339 IU/ml.
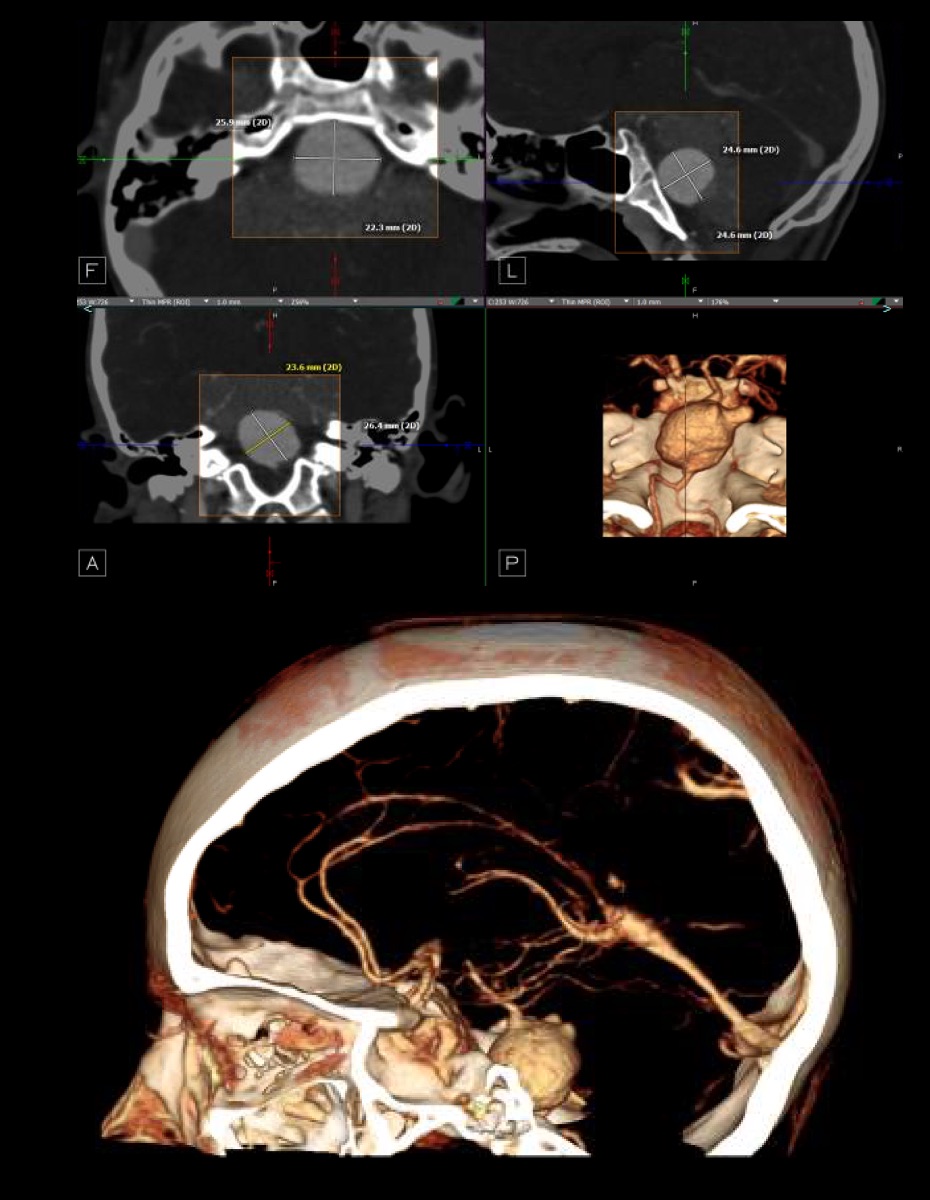
Physical examination on admission was unremarkable including no meningismus nor focal neurologic signs. Initial lab studies included an elevated WBC of 14.4 K/mm3 with 13% eosinophils. A head CT angiogram showed a large fusiform aneurysm of the mid-basilar artery measuring up to 26 mm, with a thin rim of thrombus posteriorly, a 5mm lobule projecting posteriorly, and a 1.1 cm partially thrombosed wide neck aneurysm at the right AICA origin. Neurosurgery and PICU were consulted. He was then transferred to a quaternary care children’s hospital, where he underwent embolization via the vertebral artery.
Discussion: Unlike intracranial aneurysm (IA) in adults, pediatric IA is rare, accounting for only 1-5% of all cases. Pediatric IA is more common in males; more likely to be giant, dissecting, or fusiform; more likely are found in posterior circulation and associated with spontaneous thrombosis. The most common presentation is subarachnoid hemorrhage, but due to the size of many giant aneurysms (>25mm) headache and tumor-like symptoms may be the initial presentation.
Pediatric IA is often associated with underlying congenital disease and have a higher incidence of de novo growth and recurrence as a result. Infectious etiologies are also more common, accounting for up to 15% of intracranial aneurysms in the pediatric population. Hyperimmunoglobulin E syndrome (HIES), defined as a syndrome of recurrent infections and elevated serum IgE levels, can be associated with vascular abnormalities, but IA has not been reported in patients with HIES in the literature. Our patient had features of HIES but has not been seen for a follow-up to explore the possibility of this diagnosis.
Conclusions: Pediatric IA is rare and has different underlying etiologies and presentations than adults. Children presenting acutely with signs and symptoms suggesting a tumor should be imaged immediately for possible IA. Evaluation for underlying conditions and a multi-disciplinary approach to treatment is critical.