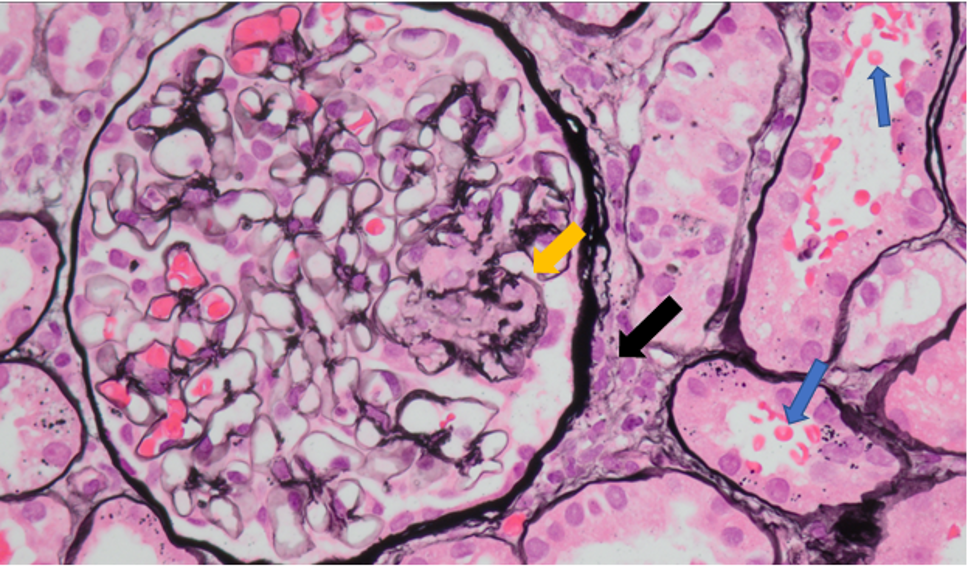
Case Presentation: A 79-year-old female nonsmoker with chronic bronchiectasis on 3 liters of home oxygen presented with worsening shortness of breath. The patient’s baseline creatinine (cr) was 0.85 mg/dL, eGFR 60, and she was admitted with cr of 2.2 mg/dL. Urinalysis showed proteinuria, pyuria, hematuria with few bacteria, with new onset anemia (Hgb 7.8) on CBC. Due to active urine sediment, worsening pulmonary status, and anemia, complement and ANCA were checked to confirm infectious glomerulonephritis vs ANCA associated vasculitis (AAV). ANCA (MPO 65.6 and SP3 24.9) returned elevated. EGD ruled out GI bleeding as a source of anemia. The patient was started on IV steroids and empiric antibiotics until respiratory cultures grew mycobacterium abscessus complex (MABC). Her MABC was previously untreated due to stable respiratory status. Her renal biopsy showed crescentic glomerulonephritis consistent with AAV. She was treated with Rituxan and prednisone and simultaneously treated with inhaled amikacin and clofazime and eventually omadocycline post insurance approval. Ultimately 2 months post discharge, patient returned with worsening shortness of breath and failure to thrive and opted to transition to comfort care.
Discussion: MABC is a nontuberculous mycobacterium (NTM) associated with infections in those with pre-existing pulmonary pathology, such as our patient with bronchiectasis. The immune response is crucial in containing MABC and immune suppression may lead to disseminated disease1. AAV is a systemic autoimmune condition which includes microscopic polyangiitis (MPA), which has preferential glomerular and pulmonary involvement and may occur secondary to MABC infection2. While AAV is a rare complication of other NTM infections, we only identified one other case report linking AAV to MABC. That case parallels our patient’s case with both patients being in their 70s, female, with MABC in the setting of bronchiectasis3. The pathogenesis of NTM infections leading to vasculitis is not well defined. However, one hypothesis suggests excess immune response to infection leads to increased ANCA antigen expression on neutrophils. Binding of circulating ANCA to ANCA antigens results in neutrophil degranulation with subsequent vascular injury. Additionally, ANCA antigens activate TGF-β, leading to promotion of fibrosis4. Given TGF-β’s inhibitory effect on TNF-α synthesis, we hypothesize this pathway may ironically also increase risk of worsening MABC infection.
Conclusions: This case highlights AAV as a rare complication of MABC, and differential for pulmonary symptoms and urine sediment in patients with chronic bronchiectasis. Treating these together requires a balance between immune suppression and adequate immune response to contain MABC and managing the complexities of chronic antibiotic therapy.