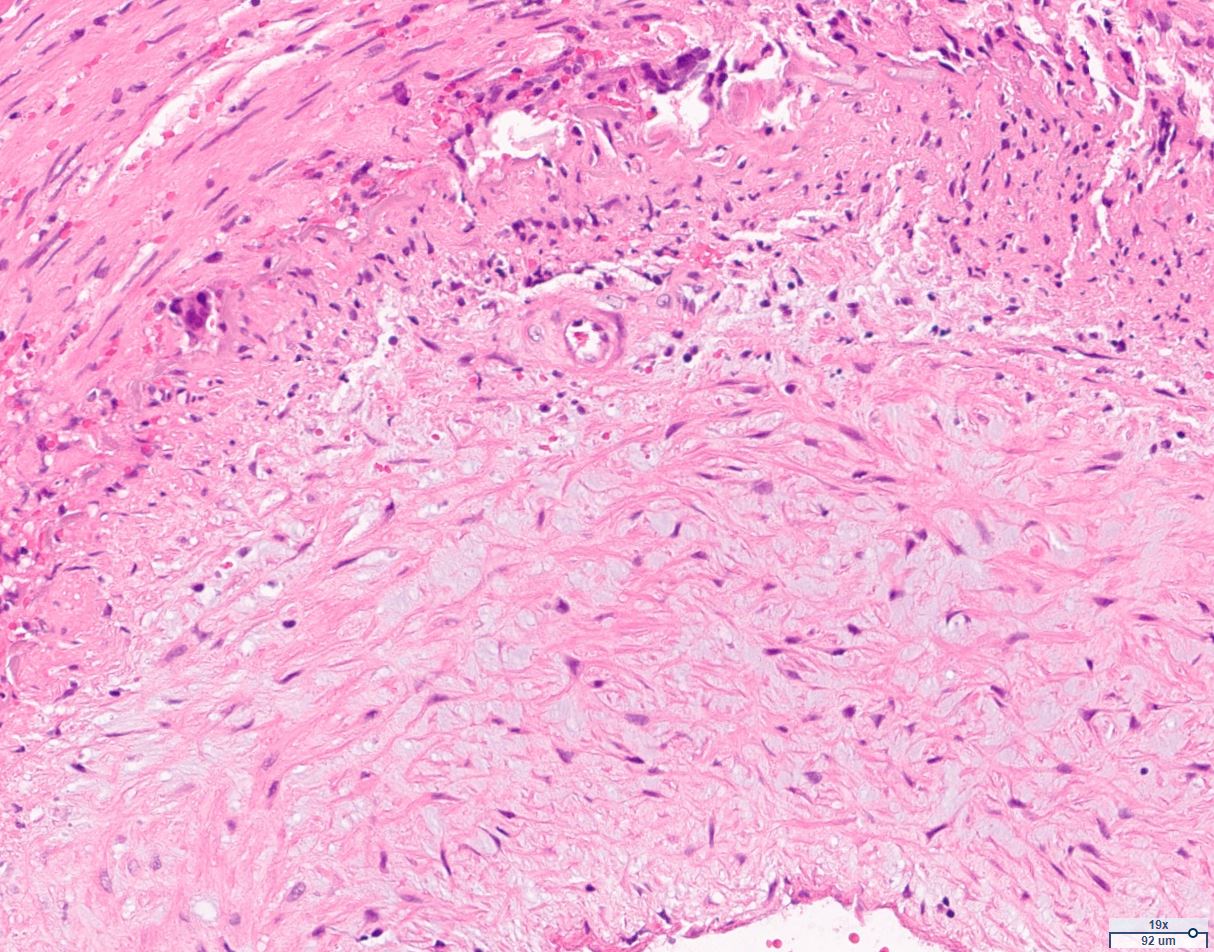
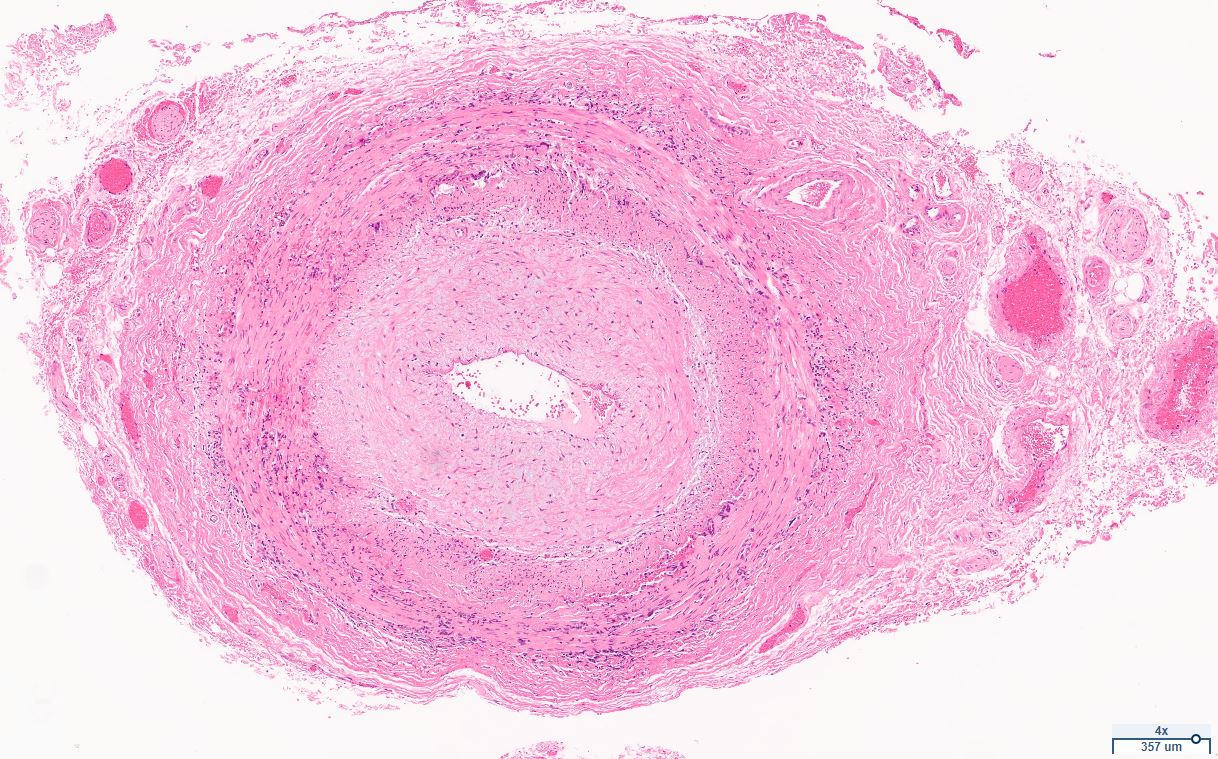
Case Presentation: An 80-year-old female was admitted with sudden right-sided weakness, expressive aphasia and left partial loss of vision. She denied preceding temporal tenderness, jaw claudication, headaches, history of tick bites, and new rashes. While her weakness and aphasia resolved within an hour, her vision impairment persisted. Initial CT and MRI scans showed no acute brain abnormalities. Laboratory tests revealed ESR 30 and CRP 2.3. An ophthalmic examination indicated left optic disc edema and an inferior visual field defect, suggestive of ION. Visual Acuity in both eyes was 20/20. Optical Coherence Tomography revealed significant swelling in the left eye retinal nerve fibre layer. Given her age, symptoms of TIA, elevated CRP, and optic neuropathy, she was started on pulse dosed steroids. Temporal artery biopsy eventually confirmed GCA, evidenced by mononuclear inflammation and giant cells in the arterial wall, along with fragmentation of the elastic laminae. Furthermore, she tested positive for Lyme disease (positive ELISA and 5 IgM bands on Western Blot). A silver stain performed to check for spirochetes was negative. Due to concern of Lyme disease causing the visual loss, she was discharged on 4-week antibiotic course (2 week IV ceftriaxone followed by oral doxycycline) and a steroid taper starting at 40mg daily. Her vision did not worsen but remained the same. A repeat examination after completing antibiotics revealed resolution of optic disc edema. To reduce the risk of recurrence and further vision loss, she was started on tocilizumab (IL-6 antagonist), accompanied by a rapid steroid taper.
Discussion: Our patient’s initial presentation was unusual for GCA with TIA in addition to vision loss. The positive test for Lyme disease raises the question of whether this presentation was related to the infection. However her TAB did return positive with classic findings of GCA. There are case reports showing GCA like symptoms and positive biopsies in the setting of Lyme infection; one of them showed a positive spirochete in the biopsy. [1,2]. However it is unclear whether the GCA is directly caused by Lyme, or if the infection triggers the cascade that leads to the vasculitis.
Conclusions: We report this case where AION secondary to GCA was associated with Lyme neuroborreliosis. Optic disc edema did improve after antibiotic course but patient’s vision did not fully recover, indicating underlying vasculitis. [3,4,5]. Spirochaetal infections should be considered when evaluating patients for GCA.