Background: Across the field of Hospital Medicine, there is a “call to arms” to build robust faculty development programs(1). Medical education and clinical teaching are common career interests for early career hospitalists (ECH), defined as hospitalists ≤5 years since postgraduate training. ECH often pursue academic positions to explore an interest in medical education, but find themselves on uncovered services with few teaching opportunities and little time or incentive to build their teaching skills in systematic faculty development programs. One potential strategy to address both of these issues is a passport program. Passports, which have been implemented in UME and GME, ensure that expectations for program participation are met, while also promoting self-directed learning, but have not been widely described for the purposes of faculty development at the attending level.
Purpose: The aim of our project is to build a medical education passport for ECH within our group based on pairing currently available education faculty development opportunities at our institution with the self-identified educational needs of these providers. Once implemented, the passport program will be used to stratify ECH for allocation of teaching service time.
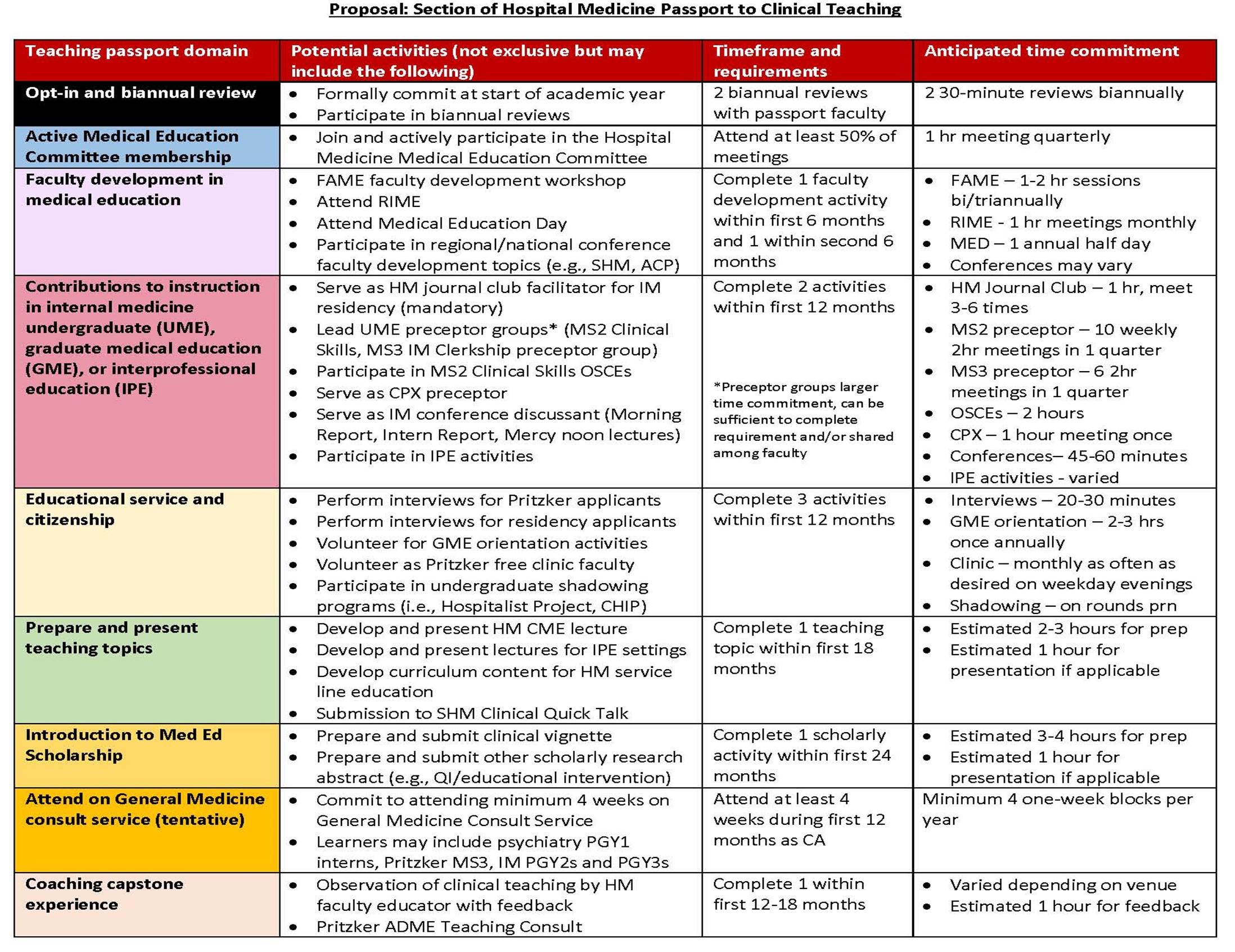
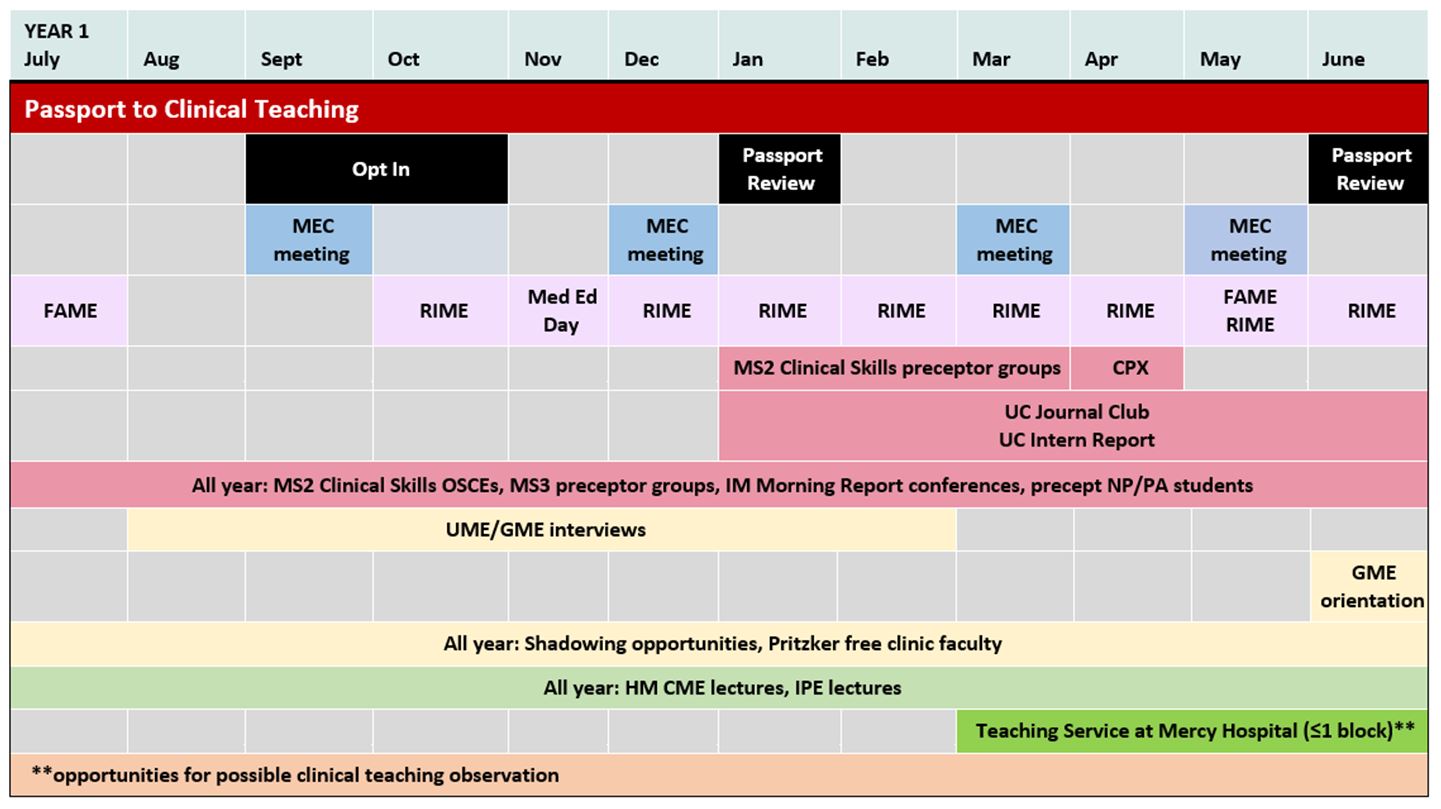
Description: Our academic Section of Hospital Medicine hired 27 new ECH in the summer of 2019. The expansion coincided with a significant increase in the number of direct care service lines, with virtually no increase in teaching service time, decreasing the proportional availability of teaching for our ECH. To identify the volume of providers interested in teaching and their experience, we surveyed the ECH. These individuals identified a strong interest in medical education with 16.7% being highly interested and 41.7% moderately interested in medical education, but they had limited confidence in their teaching abilities with only 8.3% reporting feeling highly prepared and 33.3% moderately prepared for clinical teaching. Based on this interest and confidence gap, the decision was made to develop a medical education passport. Medical education leaders within Hospital Medicine and throughout the institution were approached to identify faculty development, volunteer, and instructional opportunities that would be appropriate for ECH participation. These activities were divided into 8 separate categories based on intensity and expected skill development (Figure 1). Completion of these activities is being paired with faculty mentorship and semi-annual reviews to create a formal process. The “Passport to Clinical Teaching Program” is an opt-in two-year program open to all hospitalists. Participants formally commit to the program by the end of their first quarter of employment. Figure 2 provides an example of an expected schedule of activities for a Passport participant. Those who successfully complete the Passport Program will be eligible for prioritized scheduling on teaching services. The next step is creation of an online tracking tool for passport completion and pilot of the program. Ongoing data collection, teaching evaluations and tracking of career path development is necessary to determine passport effectiveness.
Conclusions: The gap between hospitalist interest in medical education and self-perceived level of preparedness to teach is an opportunity for innovation. A passport to clinical teaching has the potential to justly distribute scarce teaching service time and provide crucial faculty development to early career hospitalists.