Background: Hospitalized patients placed on contact, droplet, or respiratory isolation due to a carrier state or infection with resistant or highly communicable organisms report higher rates of anxiety and loneliness and have fewer physician encounters, room entries, vital sign records, physician and nursing notes in the chart. For these reasons, it has been hypothesized that isolation status might adversely impact patients’ ratings on provider communication, responsiveness, pain management and overall care. A smaller study supports this idea, but was not controlled for patient factors and was conducted at a hospital with narrow isolation practices.
Methods: We conducted a cross-sectional analysis of patient-level HCAHPS and Press Ganey survey results linked to administrative and clinical data for 2011 to 2016 from a single academic tertiary care hospital. Patients in any type of isolation for greater than 25% of their stay were defined as the exposure group and those not on isolation served as controls. Multivariable logistic regression, adjusted for race, gender, payor, severity of illness, length of stay and clinical service, was used to examine associations between isolation status and “Top-box” scores (the most positive responses) for the survey items.
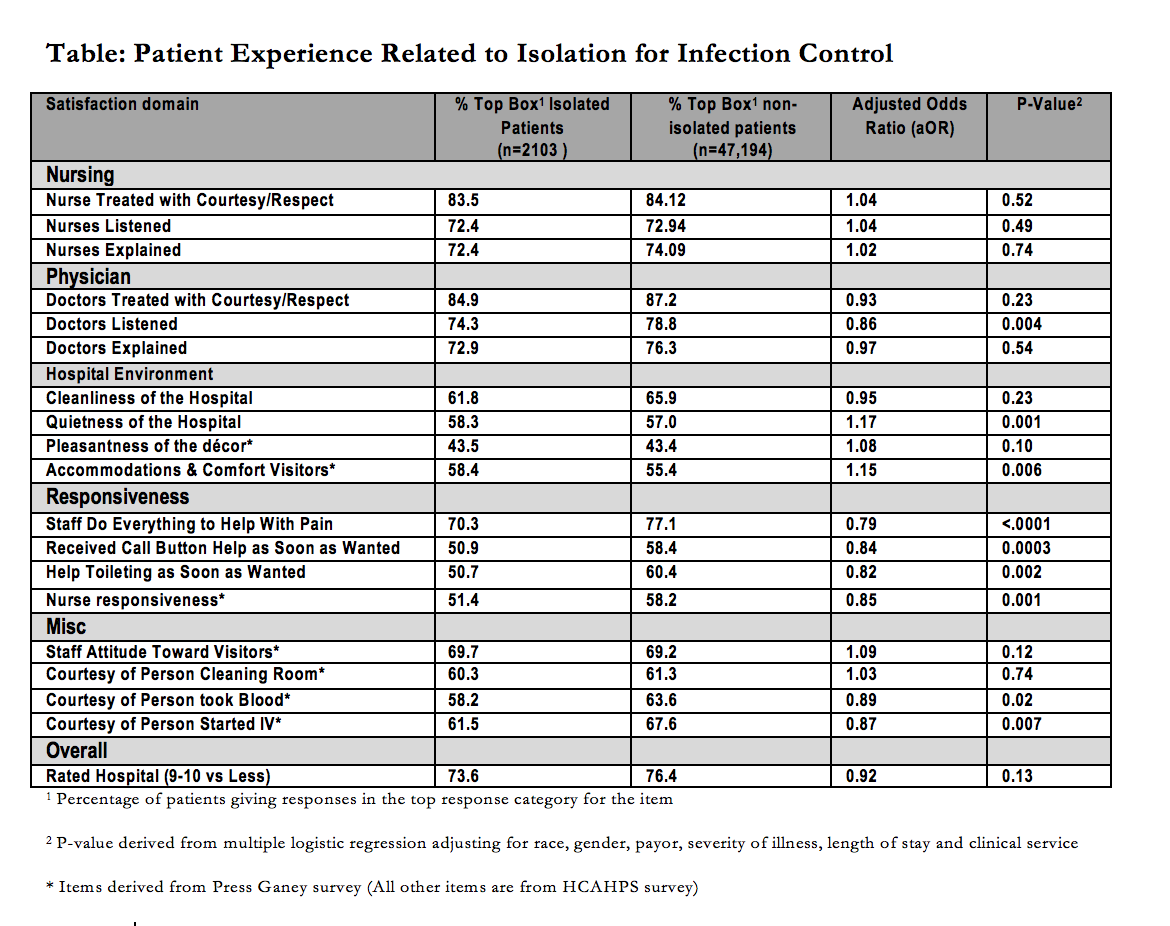
Results: Of 49,297 patients included, 2103 were in isolation. Other than “Doctors Listen Carefully” (aOR 0.86, p=0.004), patient experience with nursing, physicians and overall care was not significantly different between the groups. Isolated patients reported worse experience on several items related to staff responsiveness: pain control aOR 0.79, p<0.0001; call button help aOR 0.84, p=0.002), but better experience with quietness (aOR 1.17, p=0.001) and visitor comfort (aOR 1.15, p=0.006).
Conclusions: Patients placed in isolation do not report adverse experience for most of the items related to provider communication. This is reassuring since the communication items are regarded to be some of the most important items for safety and quality of care. However, patients in isolation had worse experience with staff responsiveness for time sensitive needs related to toileting, call button help, nursing and pain control. Hospitals should increase staff awareness on this aspect of care and emphasize timely response, especially for this population. The paradoxically better experience with quietness and visitor comfort may be related to isolated patients more frequently being assigned to private rooms.