Background: The US faces a worsening epidemic of substance use-associated morbidity and mortality. In 2021, over 46 million people had a substance use disorder (SUD) and over 109,000 overdose deaths occurred. Furthermore, an estimated 1 in 7 hospital admissions are for patients with SUDs. Stigma is pervasive among these patients’ hospital providers, and SUD management during medical admissions is often inadequate. Little is known about how patients with SUDs perceive their care quality, are impacted by stigma in hospital settings, or how they would recommend improving care. In this qualitative study, we seek to identify perspectives on positive aspects, negative aspects, and consequences of care, as well as recommendations for improvement among hospitalized patients with SUDs.
Methods: We conducted a qualitative descriptive study at an urban academic hospital, utilizing convenience sampling to recruit adults with an SUD diagnosis admitted to medical or surgical floors. We carried out semi-structured, in-depth interviews during the patients’ hospital admissions exploring their experiences during the present and prior hospitalizations. The interviews were audio-recorded, transcribed, then analyzed in NVivo. Two analysts coded the transcripts using an inductive approach according to grounded theory. Interviews were conducted in tandem with thematic analysis and continued until theoretical saturation. Demographic and clinical data were analyzed with descriptive statistics.
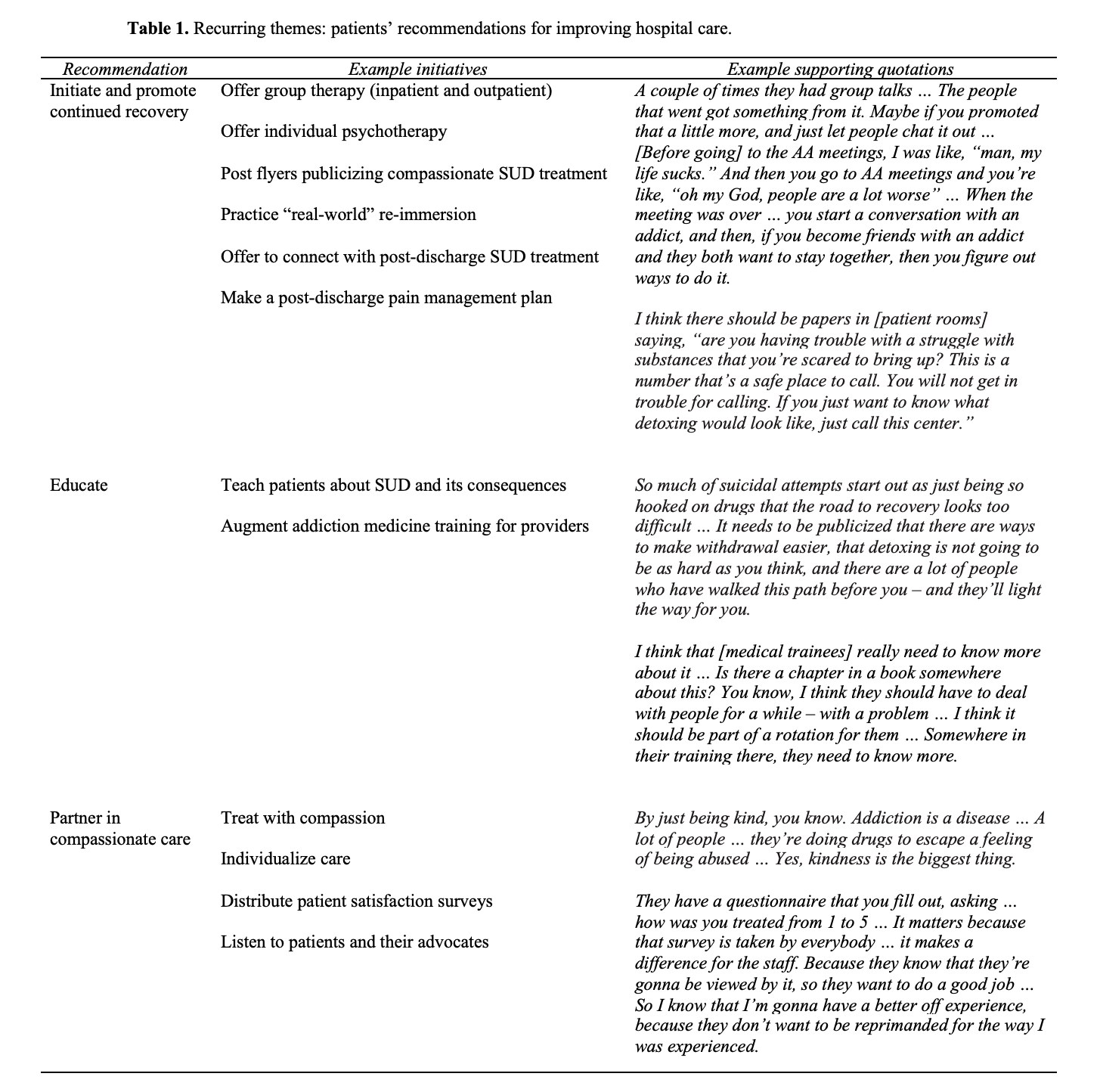
Results: We interviewed 15 patients. Their median age was 58 (range 25-74). Eleven (73%) were housed and 4 (27%) were unhoused. Eight (53%) had opioid use disorder, 8 (53%) had alcohol use disorder, 4 (27%) had stimulant use disorder, 3 (20%) had tobacco use disorder, 1 (7%) had benzodiazepine use disorder, and 6 (40%) had more than 1 SUD. Qualitative analysis revealed 2 recurring themes that defined positive aspects of care: perceived clinical proficiency — including partnership, knowledgeability, ethics, and adequate care delivery; and perceived emotional proficiency — including compassion and investment in relationships. Three recurring themes defined negative aspects of care: perceived bias and stigmatized attitudes — including assumptions, labeling, and judgment based on substance use history; perceived clinical improficiency — including lack of partnership, poor knowledge, and inadequate care delivery; and perceived inhumane treatment — including disrespect, neglect, and discrimination based on substance use history. These aspects of care were most consequential for patients’ emotional wellbeing, trust, confidence in care, and quality of pain and withdrawal management. Patients recommended specific approaches to improve care by initiating and promoting continued recovery, educating, and partnering in compassionate care.
Conclusions: Our study highlights under-recognized perspectives from hospitalized patients with SUDs, including emphases on compassion and investing in partnerships to address patients’ needs, as well as consequences of care for patients’ emotional wellbeing, trust, and health outcomes. Patients offered novel recommendations for improving care that warrant further investigation. Future studies will be needed to characterize perspectives of patients from different demographic backgrounds and clinical settings. By striving to advance our care in accordance with patients’ viewpoints, we can turn hospitalizations into opportunities for engagement and promoting recovery.