Background: Acute pancreatitis (AP) is one of the most common causes of hospitalization in the United States. Intravenous hydration with normal saline (NS) is the most commonly used fluid for resuscitation. Recent studies have shown better outcomes with the use of more pH balanced fluid-like ringer’s lactate and Plasmalyte (PL). We conducted a retrospective cohort study to evaluate the differences in outcomes of AP in patients who received NS compared to PL.
Methods: All patients >18 years of age admitted to our hospital with the diagnosis of AP from November 2016 to October 2018 were included in the study. Primary outcomes were persistent systemic inflammatory response syndrome (SIRS) at 48 hours and mortality. Secondary outcomes were readmission within 30 days and length of stay (LOS). Categorical characteristics of NS and PL patients were compared using Pearson’s chi-square or Fisher’s exact tests and continuous ones were compared using Student’s t-tests or Wilcoxon rank-sum tests. Statistical analysis was conducted using SAS 9.4.
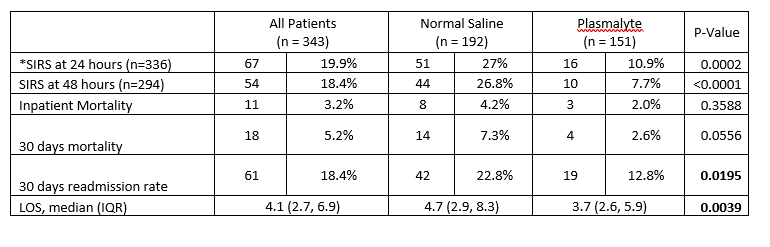
Results: Three hundred forty-three patients met our inclusion criteria, 192 patients received NS, and 151 received PL for intravenous hydration. Persistent SIRS at 48 hours was significantly higher in patients who received NS compared to PL (26.8% vs. 7.7%; P=<0.0001). LOS was significantly higher in patients who received NS (4.7 days vs. 3.7 days, P=0.0039). Thirty days readmission rate was also significantly higher in the NS group (22.8% vs. 12.8%; P=0.0195). Mortality although trended lower in the PL group, was not statistically significant (7.3% NS group vs. 2.6% PL group, P=0.0556). In multivariable analysis use of PL is associated with lower odds of 30 days readmission [OR=0.515 (CI:0.280 - 0.950); P=0.0338] and shorter LOS [%decrease=16.6% (CI: -26.4%, -5.5%); P=0.0045].
Conclusions: Our study revealed that the use of PL in AP is associated with a lower rate of persistent SIRS at 48 hours, shorter LOS, and lower 30 days readmission rate. There may also be a mortality benefit with the use of PL, for which larger randomized controlled are needed.