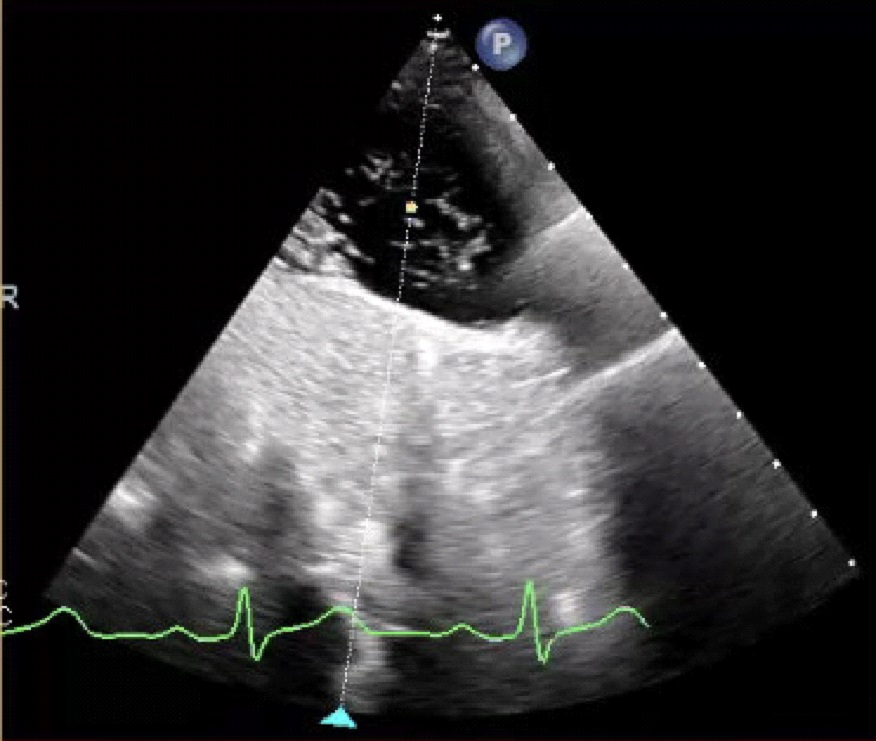
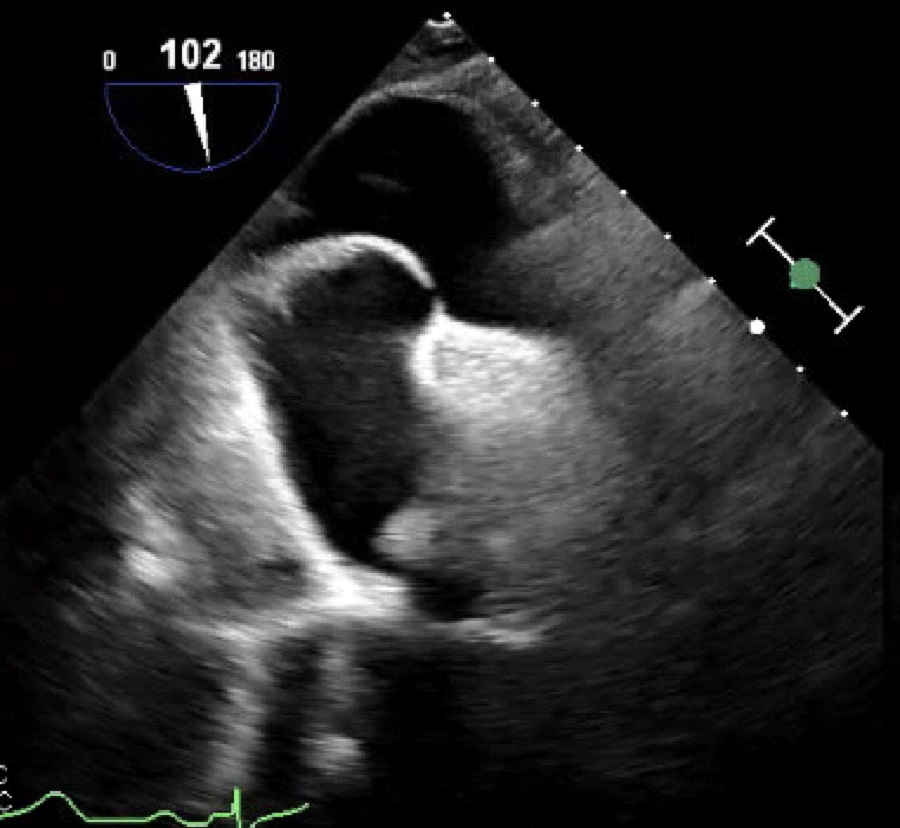
Case Presentation: An 86-year-old man with a history of stroke on apixaban and metastatic renal cell carcinoma on ipilimumab/nivolumab presented to our emergency room with lightheadedness. Transthoracic echocardiogram (TTE) for stroke evaluation performed 3 years prior revealed a patent foramen ovale (PFO). Vital signs were significant for hypoxemia to 85% on room air requiring high-flow nasal cannula at 100% FiO2 to maintain oxygen saturation >90%. CT scans showed hemoperitoneum due to bleeding metastasis and normal pulmonary parenchyma without pulmonary embolism. TTE demonstrated a left ventricular ejection fraction of 71% and early passage of bubbles from the right to left atrium consistent with an intracardiac shunt. Transesophageal echocardiogram confirmed brisk right to left shunting consistent with a PFO. Hypoxia resolved with supine positioning and recurred with sitting upright or standing, consistent with platypnea-orthodeoxia syndrome (POS). Orthostatic hypotension was also noted.Due to hemorrhage found on admission, percutaneous closure of the PFO was deemed to be prohibitively high-risk due to need for uninterrupted dual-antiplatelet therapy. His functional capacity was limited due to orthostatic hypotension and orthodeoxia. Midodrine was started to increase left atrial pressure to decrease shunt fraction. An initial dose of midodrine 5 mg three times daily showed partial response and an increased dose of 10 mg three times daily resulted in resolution of orthodeoxia. Oxygen saturation improved on discharge when upright from 81% to 92% after initiation of midodrine. Due to progression of malignancy, cabozantinib was started which resulted in new-onset severe hypertension. This required cessation of midodrine and the patient developed recurrent orthodeoxia requiring admission. Although his symptoms again responded to midodrine, HTN management became a central concern to rechallenge cabozantinib.To improve tolerance of cabozantinib, a percutaneous PFO closure was performed 8 months after presentation. Right atrial pressure was 7 mmHg and mean pulmonary artery pressure was 15 mmHg. A post-procedural TTE demonstrated trivial residual shunting through the PFO. However, orthodeoxia resolved and midodrine was discontinued 5 weeks later.
Discussion: Platypnea-orthodeoxia due to PFO is rare. Although autopsy series reveal PFO in around 1 out of 4 hearts, POS due to PFO is mainly limited to case reports.1 Case series have shown an association of POS due to PFO with atrial septal aneurysms similar to this patient.2,3In this case, POS due to intracardiac shunting from a PFO was successfully treated with oral midodrine in a patient at prohibitive risk for procedural intervention. Midodrine initiation was temporally associated with improvement of hypoxemia and stopping midodrine was associated with recurrence.This is the second reported case on the use of midodrine to treat POS due to PFO. In the prior case, midodrine and fludrocortisone were used for 3 months until symptoms progressed through medical management necessitating closure.4Further research is needed to determine the long-term safety of medical management of POS due to PFO. In most cases, percutaneous closure of the PFO remains standard of care due its high success rate.5,6
Conclusions: Midodrine may be a well tolerated treatment option for patients with platypnea-orthodeoxia syndrome due to patent foramen ovale who are not candidates for percutaneous closure.