Background: The Centers of Medicare and Medicaid (CMS) in 2024 will require hospitals to screen and report two of the following five health-related social needs (HRSN): food insecurity, housing instability, transportation needs, utility difficulties, and interpersonal safety (1). These regulations improve screening, however, institutions are still left with questions on how to address these HRSN, including what populations could participate in the solution.
Purpose: To create an inpatient pre-professional health program that can screen and address HRSN for patients along with training the next generation of health care providers and giving them an opportunity to get meaningful direct patient care.
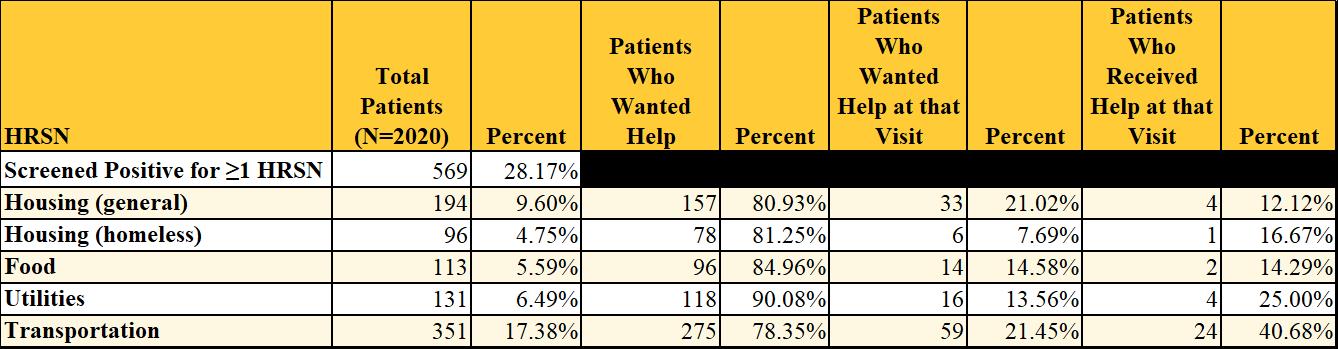
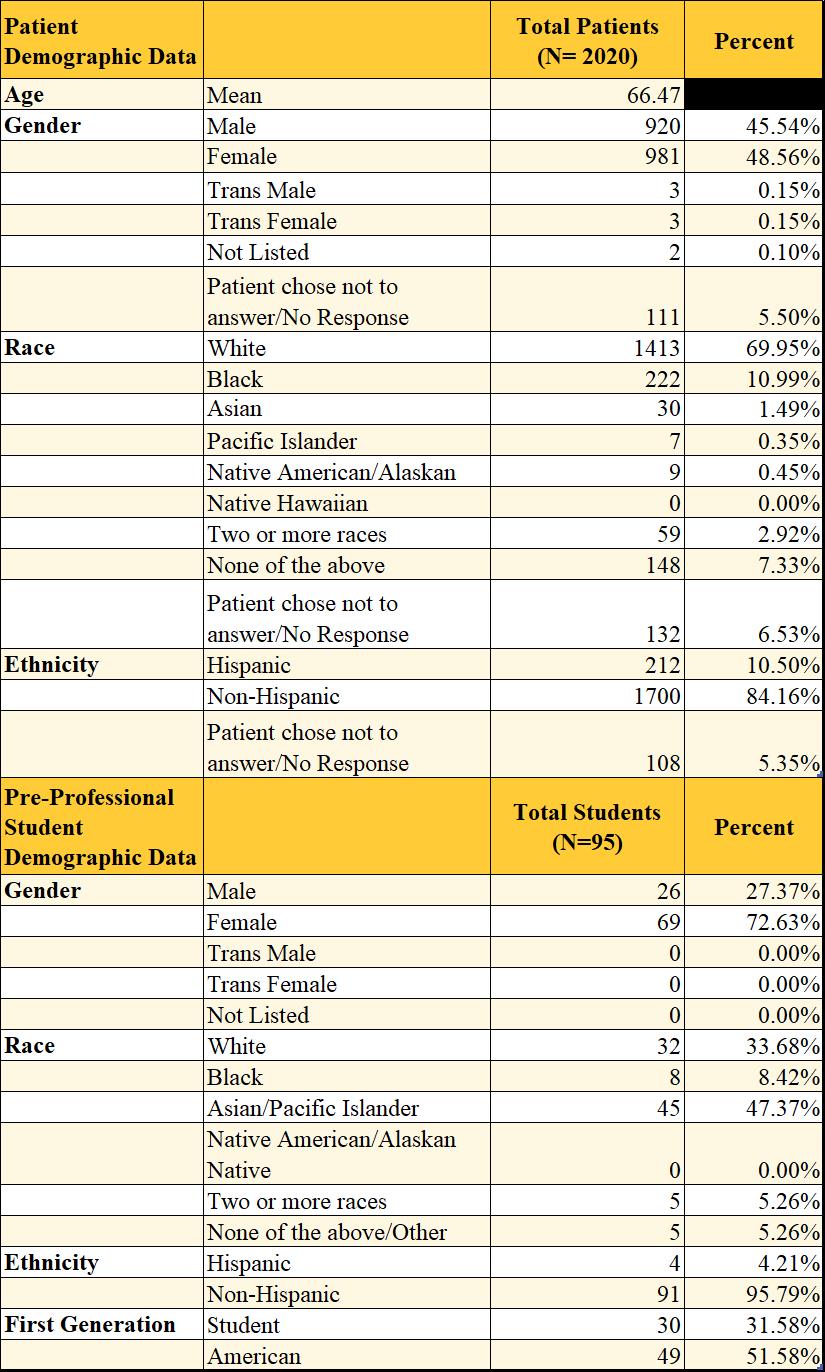
Description: Using the PRAPARE screening tool, we utilized pre-professional health students to screen patients while admitted to John Dempsey Hospital for food insecurity, housing instability, transportation needs and utility difficulties. All patients who were positive for any HRSN were offered community resources through a warm handoff method. All patients were eligible for screening except those < 18 y/o, altered mental status, on airborne precautions, from the Department of Corrections, or in the ICU. Between September 2021-August 2023, 95 pre-professional students screened 2020 patients, of which 569 screened positive for 1≥ HRSN with an average positivity of 1.72 HRSN. Of that population, 17.38% lacked transportation, 6.49% experienced utility difficulties, 5.59% were food insecure, 9.6% faced housing instability, and 4.75% were homeless. Of the 351 patients who lacked transportation, 78.35% were interested in being connected to a resource and 21.45% wanted to be connected at that visit. Of those that wanted to be connected, 40.68% were successfully connected. Of the 118 patients experiencing utility difficulties, 90.08% were interested in connecting to a resource, 13.56% wanted to be connected at that visit and 25% were successfully connected. Of the 113 food insecure patients, 94.96% were interested in connecting to a resource, 14.58% wanted to be connected at that visit and 14.29% were successfully connected. Of the 194 patients with housing instability, 80.93% were interested in connecting to a resource, 21.02% wanted to be connected at that visit and 12.12% were successfully connected. Of the 96 patients facing homelessness, 81.25% were interested in connecting to a resource, 7.69% wanted to be connected at that visit, and 16.67% were successfully connected.
Conclusions: Students interested in medical careers can effectively screen and address health-related social needs of admitted patients in the hospital. Hospitalized patients report high frequencies of HRSN and a desire to address their needs. Those with transportation difficulties showed the highest interest in addressing them during their visits, meaning they may have found this need the greatest at the time. Factors such as extreme illness or not having information on hand to fill out resource applications may influence their decisions to accept resources for other HRSN, however, further research is needed to better understand why patients are declining opportunities to be connected to resources. As hospitals develop their screening programs, they should consider utilizing the pre-professional health student population to address unmet social needs.