Background: Given that nearly 1 in 3 patients are readmitted to the hospital within 90 days of admission for acute exacerbation of COPD (AE-COPD), efforts exist to develop tools to better identify patients at higher risk for readmission. Our group has previously published a model based on International Classification of Disease, Ninth Revision and Tenth Revision, Clinical Modification (ICD-9-CM, ICD-10-CM) for predicting 90-day readmission risk after AE-COPD hospitalization that performed with an AUC of 0.74. However, ICD administrative codes for identifying AE-COPD pose potential limitations for accurate identification of AE-COPD admissions. Therefore, we sought to compare the performance of a model for predicting readmission within 90 days trained on administrative data against a model trained on a gold-standard cohort of patients identified with manual chart review.
Methods: Chart reviews of patients hospitalized at a single institution between 2008 and December 2018 that were 40 years or older at admission along with AE-COPD ICD-9-CM codes and/or AE-COPD medications were reviewed. A structured definition utilizing prior history of lung disease, mention of AE-COPD in the discharge summary, medications received, and discharge diagnoses was used to assign a categorical probability (definitely not, probably not, possibly, probably, definitely) that each index admission was truly caused by AE-COPD. Admissions that were classified as “probably” or “definitely” were ultimately chart reviewed to determine whether the patient truly presented with AE-COPD. Patient comorbidity burden was assessed using the Elixhauser Comorbidity Index. A random forest model constructed with variables including patient demographic information (age, gender, race), comorbidities, lab values, and vitals was trained using 70% of the patients confirmed to have AE-COPD. The DeLong test was used to compare model performances of the chart review and previously published administrative model were assessed using the other 30% of patients confirmed to have AE-COPD.
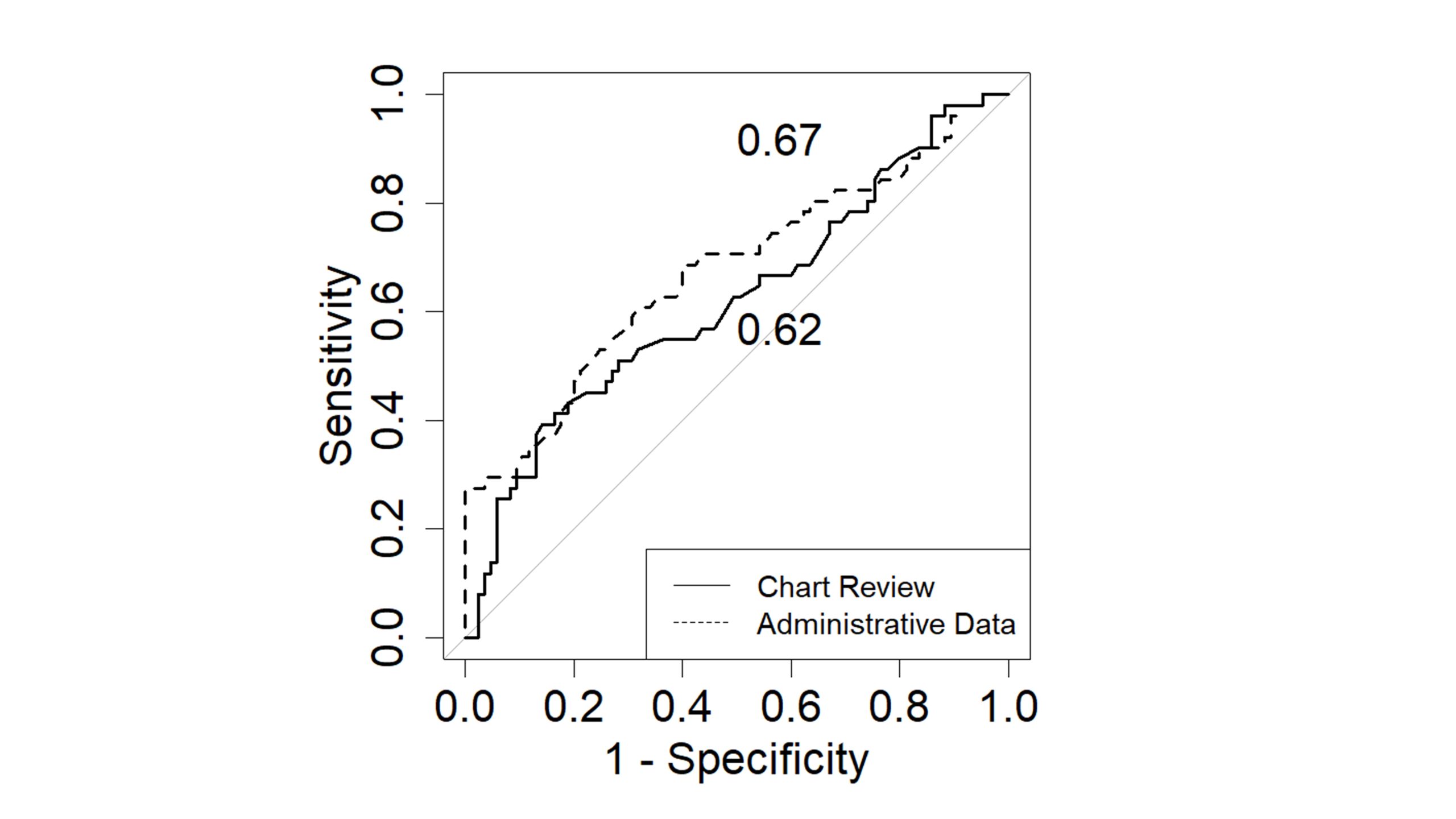
Results: Of 3,730 total admissions, 452 admissions were confirmed to be for AE-COPD by chart review. Of these patients, 38% (174) were readmitted within 90 days. A majority of patients were female and black with an average age of 62 years. There were no significant differences in the demographic characteristics of patients who were readmitted compared to those who were not. Patients who were readmitted had greater comorbidities on average with a higher Elixhauser Index (12.5 vs. 9.8, p=0.03). The random forest AUC for the administrative data model was 0.67 while the AUC for the chart review model was 0.62 (p=0.4). (Figure)
Conclusions: Our results suggest that our previous model trained on patients identified using ICD codes was not inferior in performance compared to training on patients identified using manual chart review. Given the resource intensive process of manual chart review, our results provide promise to the validity of developing further tools to predicting COPD readmission risk using administrative data.