Background: Patients who are hospitalized for a prolonged period are at risk of developing various complications, includingfeeding intolerance resulting from reduced gastrointestinal motility. Prucalopride is one of the drugs used for thetreatment of constipation, and it exerts its effects by increasing intestinal motility through the activation of the 5-HT4receptor.However, no previous study demonstrated whether prucalopride was effective for delayed gastric emptying treatmentfailure by conventional prokinetics, especially feed intolerance We aim to indirectly evaluate the improvement offeeding intolerance by administration of prucalopride, monitoring the intake volume. and defecation time.
Methods: A retrospective analysis was performed for the tube-feeding in-patient who received prucalopride for treatment of feed intolerance. A total of 1002 patients were treated by prucalopride during their admission From October 2018 to January 2023 at Inha University Hospital. Among them, 194 patients received tube feeding due to their co-morbidity. And we excluded 34 out-patients describing prucalopride. Finally, we collected 137 tube-feeding patients (90 male and 47 female)/.. To investigate the change of intake amount, we analyzed the amount of intake from pre-administration day to two days after administration., We utilized the Wilcoxon signed-rank test, a non-parametric test to compare the amount of intake.
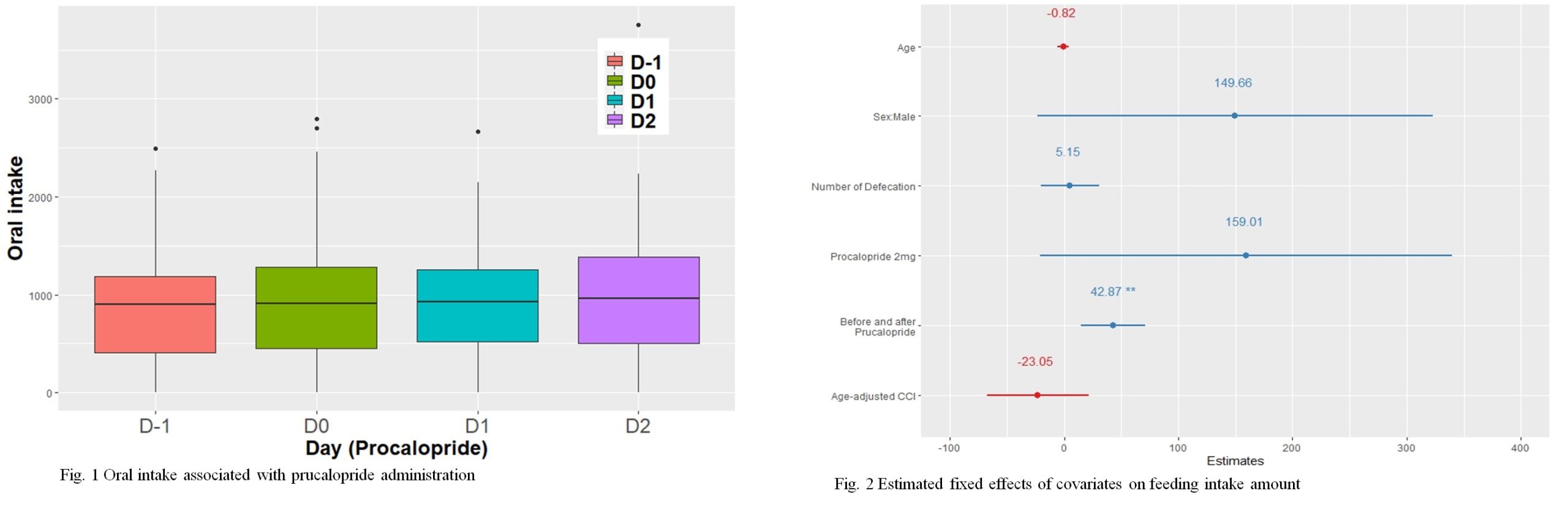
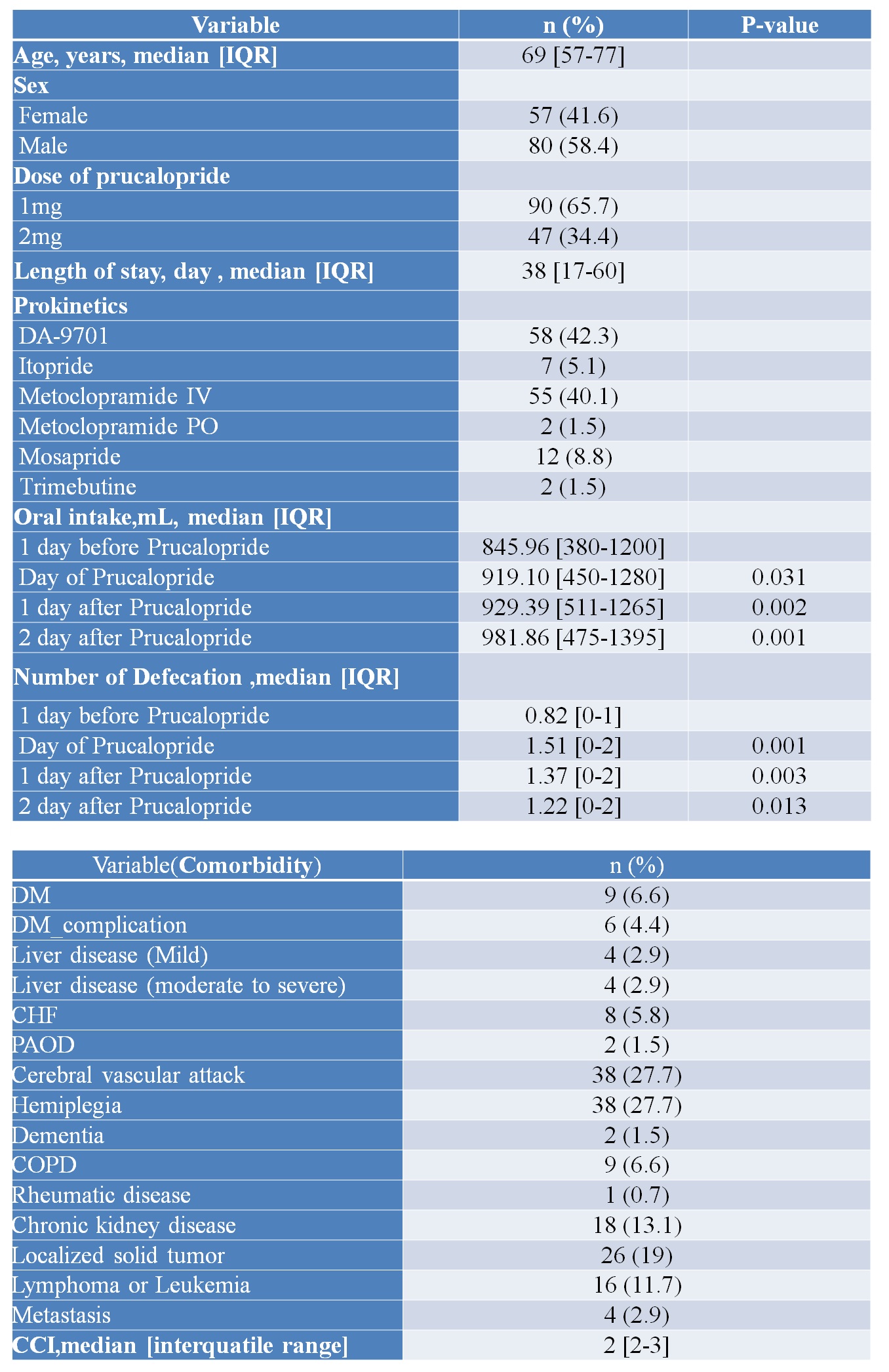
Results: Before the administration, the median intake volume was 845.96ml (interquartile range[IQR], 380.0-1200.0) and this increased gradually to 919.10ml (IQR, 450.0-1280.0) on the day of administration, 929.39ml (IQR, 510.5-1265.0) on the next day after administration, and 981.86ml (IQR,475.0-1395.0) on the second day after administration. The change of intake compared to the pre-administration day were significantly increased (P=0.031, 0.002, and 0.001, respectively). Similarly, the defecation frequency increased from 0.82 (IQR, 0.0-1.0) times before administration to 1.51 (IQR, 0.0-2.0) times on the administration day, and to 1.37 (IQR, 0.0-2.0) and 1.22 (IQR, 0.0-2.0) times on the first and second day after administration, The change of defecation number compared to the pre-administration day were significantly increased (P=< 0.001, 0.003, and 0.013, respectively)
Conclusions: Salvage therapy with prucalopride may effectively improve the delivery of nutrition for patients with feeding intolerance.Further large and multi-center prospective studies were needed.