Background: Overuse of non-ICU continuous cardiac (telemetry) monitoring is a well-documented problem that leads to increased hospital cost, alarm fatigue, nursing time loss, and patient discomfort. It is often ordered for detection of clinical deterioration or higher level of nursing care, without corroborating evidence. Several studies have looked at different interventions to reduce inappropriate telemetry use with varying success. Given the persistence of unnecessary telemetry use, it may require a multimodal intervention to effectively change institutional ordering habits.
Methods: We instituted a multimodal campaign to reduce inappropriate telemetry use within the non-teaching hospitalist services at a large urban academic hospital. The sequential interventions included didactic sessions, educational posters, utilization of a pre-existing electronic health record (EHR) silent indicator, and reminder pages. We retrospectively reviewed telemetry orders placed by hospitalist providers during the pre-intervention period (Jun – Nov 2017), intervention period (Dec 2017 – Nov 2018), and last 6 months of intervention (Jun – Nov 2018). We also prospectively monitored daily telemetry use from January to November 2018, with intermittent sampling.
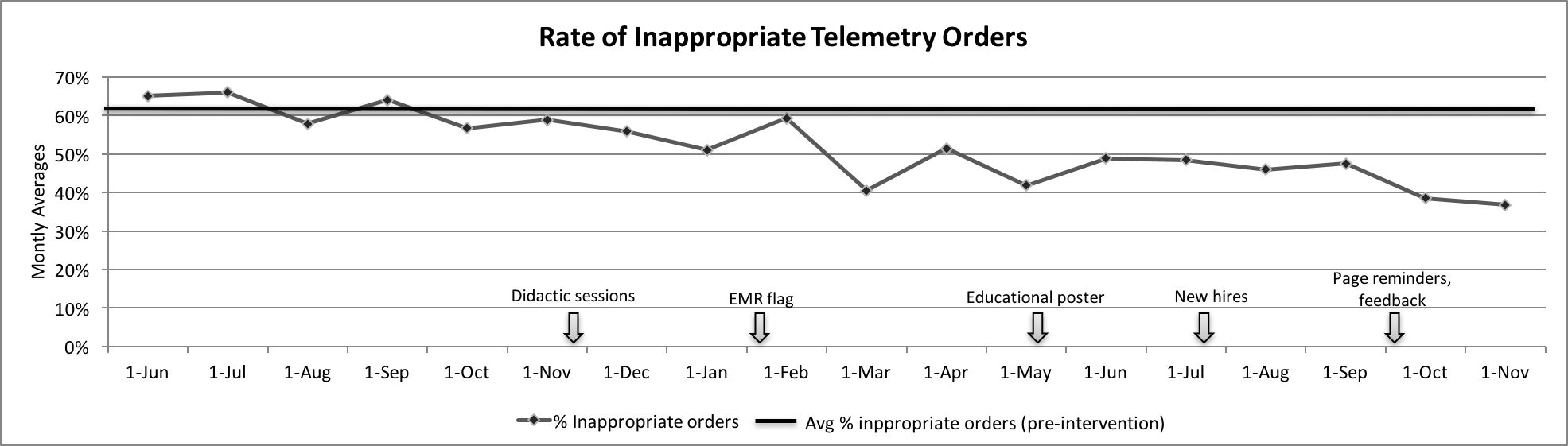
Results: A total of 2324 telemetry orders between July 2017 and November 2018 from 57 hospitalist providers were reviewed. There was a 27% decrease of monthly average percent of inappropriate orders from the pre-intervention period to the last 6 months of intervention (61% to 44%, p=0. 001, Figure 1). The monthly average duration of telemetry order decreased from 98 to 88 hours between the pre-intervention and intervention period, p=0.026. A run chart of daily percentage of patients on telemetry from January to November 2018 showed 3 downward shifts corresponding to the introduction of the EMR silent indicator, educational poster, and page reminders. We did not have pre-intervention data of daily telemetry usage rates, thus used the surrogate average from Jan 2018 for baseline comparison. The percentage of patients on telemetry appeared to trend up between interventions and with the introduction of new providers who were not exposed to previous interventions (Figure 2).
Conclusions: Inappropriate telemetry use among hospitalist providers at a large academic center can be reduced with an aggressive multimodal campaign utilizing high-yield educational materials, an EMR silent indicator, and page reminders. However, sustainability may be difficult with the yearly flux of new providers and requires motivated personnel to track and maintain section awareness of telemetry utilization.
.png)
