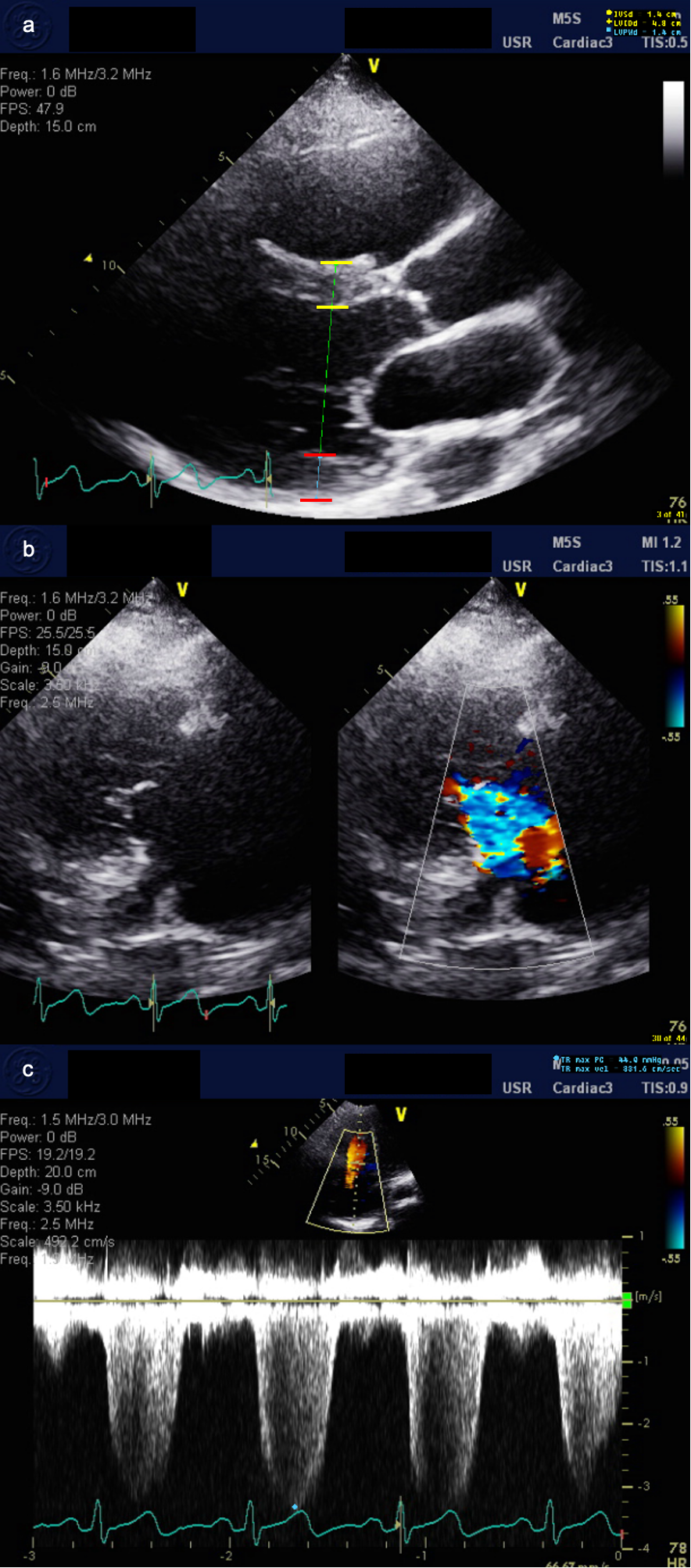
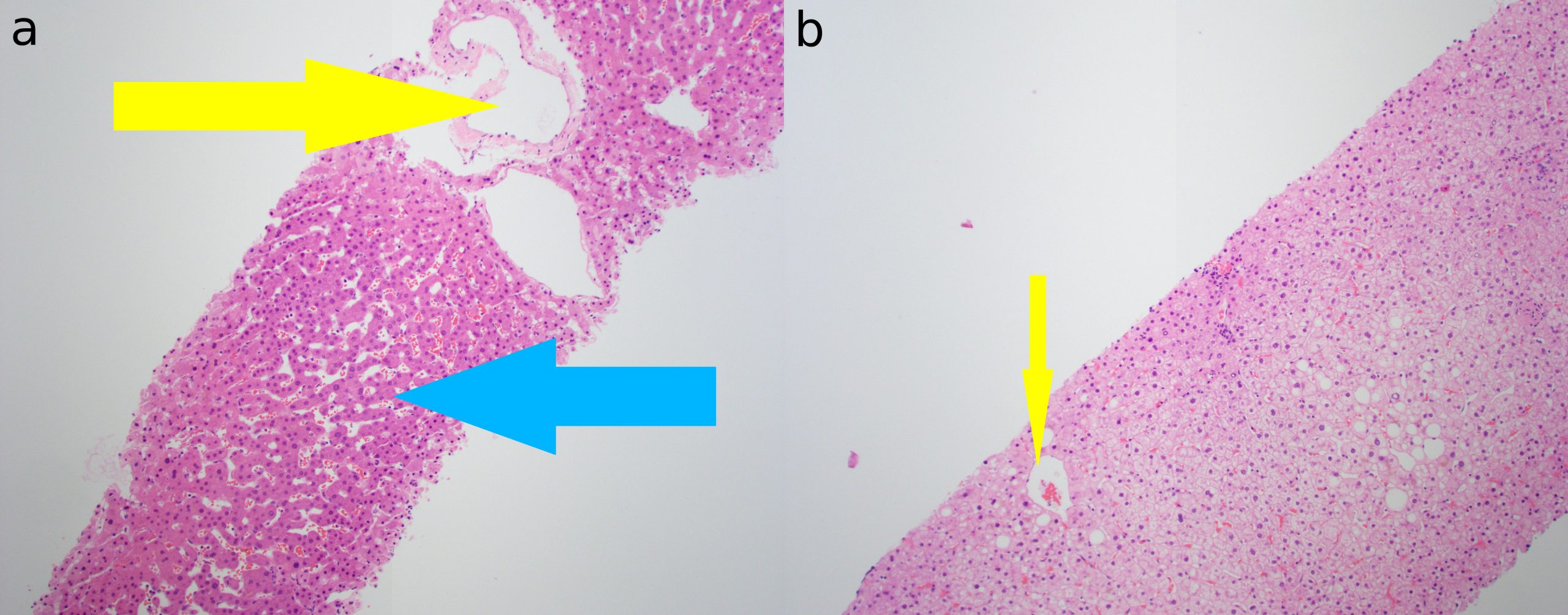
Case Presentation: A 44-year-old African American female with a medical history of chronic heart failure with preserved ejection fraction (HFpEF) presented with a six month history of multiple hospitalizations for acute decompensated HFpEF and right upper quadrant pain. One month ago, she presented with an acute elevation of alkaline phosphatase (ALP) to greater than four times the upper limit of normal, which prompted extensive but ultimately negative workup for inflammatory, infectious, and autoimmune processes. This admission, the patient presented again for acute decompensated HFpEF and severe right upper quadrant pain with an elevation of ALP to almost greater than eight times the upper limit of normal. Negative findings on further extensive cholestasis workup led the team to suspect a cardiohepatic cause of cholestasis. Limited transthoracic echocardiogram (TTE) showed normal LVEF (64%), moderate tricuspid regurgitation, and moderate pulmonary hypertension consistent with prior TTE. To further work up a differential of congestive hepatopathy versus anti-mitochondrial antibody negative primary biliary cholangitis (PBC), liver biopsy was conducted. Definitive histological features of PBC were not seen. Mild dilatation of central veins and adjacent sinusoids was consistent with congestive hepatopathy. No steatosis, fibrosis, cholestasis, or inflammation was identified. Based on clinical findings and our investigations, we diagnosed this patient with congestive hepatopathy.
Discussion: Congestive hepatopathy is the manifestation of chronic passive congestion due to right heart failure. The signs and symptoms of right heart failure often predominate early presentation. Thus, patients with congestive changes often remain asymptomatic for a long time with abnormalities in liver function tests frequently being the first indicator of hepatic pathology. Liver injury due to passive hepatic congestion presents with a characteristic mild change in serum cholestatic markers of ALP, gamma-glutamyltransferase, and total bilirubin. This case exemplifies the diagnostic approach to evaluating a heart failure patient who presents with abnormal liver function. In heart failure patients with abnormal liver function, biliary or primary hepatic pathology should be evaluated before attributing liver function abnormalities to cardiac disease. The existing literature has extensively studied the impact of liver function enzymes in heart failure with reduced ejection fraction (HFrEF) with limited research on their impact on HFpEF. In both HFrEF and the limited studies on HFpEF, ALP has been generally found to be normal or mildly elevated. There are very few reports in the literature of significantly elevated ALP levels in congestive hepatopathy, and these reports are in HFrEF not HFpEF patients. After extensive literature review, to our knowledge, this patient is the first reported case of significantly elevated ALP caused by congestive hepatopathy in the setting of HFpEF.
Conclusions: Complex cardiohepatic interactions often result in the co-existence of heart failure and liver disease. A structured approach that consists of clinical, biochemical, and technical diagnostic measures is important in the evaluation of elevated alkaline phosphatase. Unexplained chronic cholestasis in the setting of congestive heart failure should raise the suspicion for congestive hepatopathy.