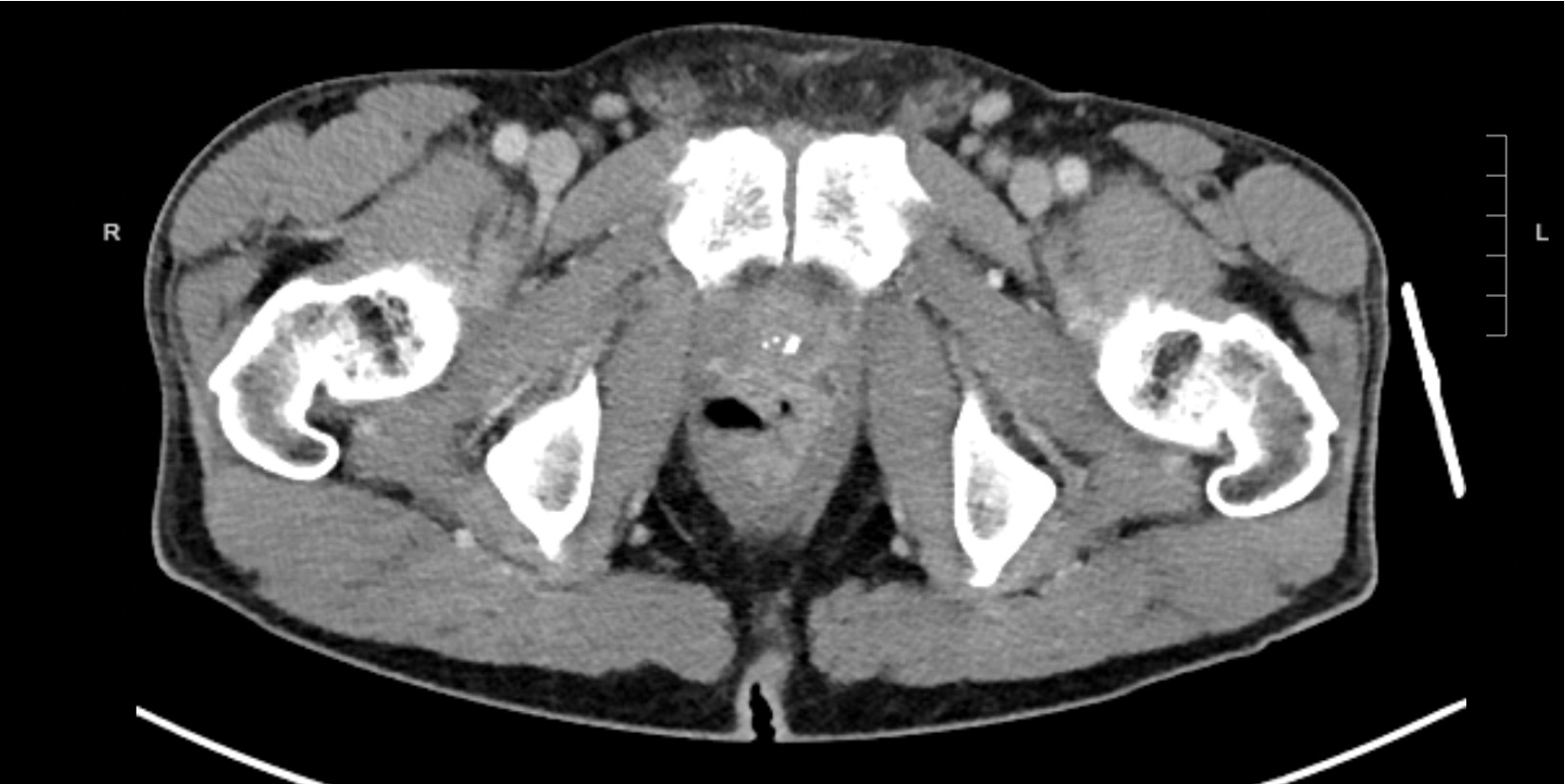
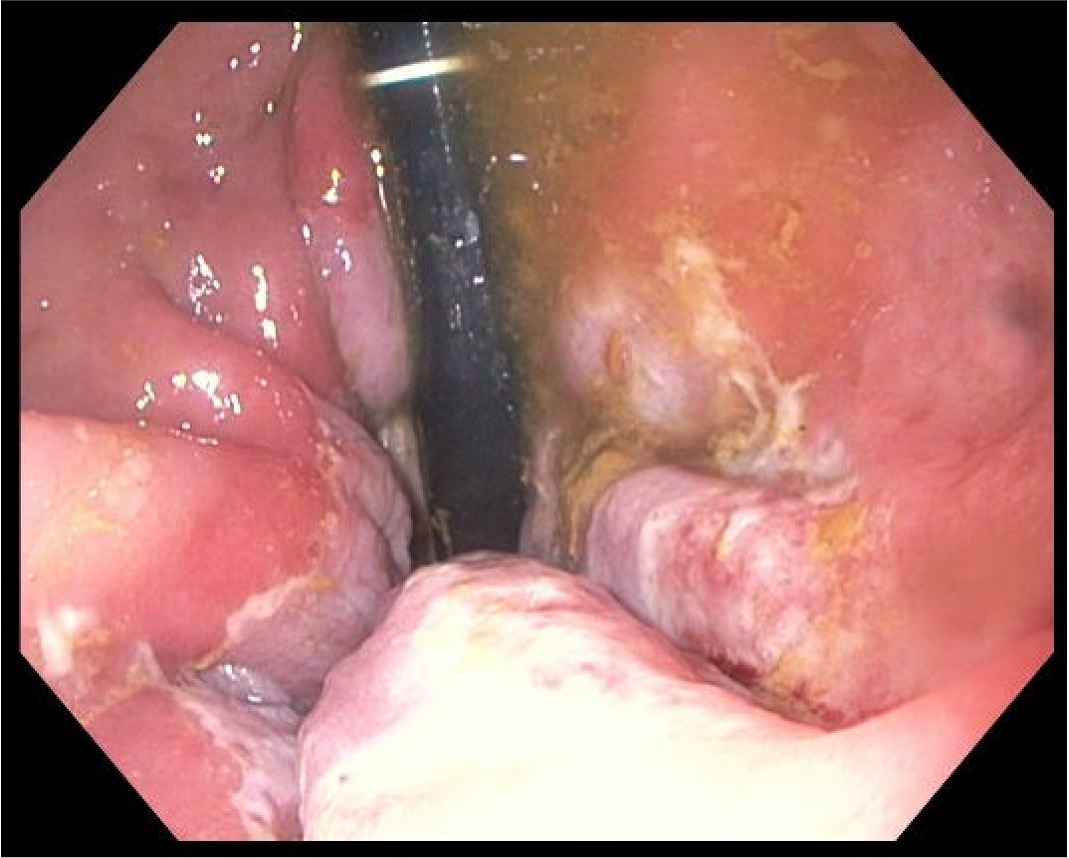
Case Presentation: A 59-year-old male with a history of HIV, HBV, and amphetamine use disorder presented with a three-day history of fever, diffuse abdominal pain, and rectal pain with passage of thick, clear-yellow fluid. The patient engaged in receptive anal intercourse and had a history of injecting methamphetamine per rectum. Patient was septic on admission with a temperature of 38.7 C, HR 116, RR 21, and WBC 16.28. CD4 count was 908 and viral load < 40 copies/mL. Proctitis was suspected given CT abdomen revealing rectal wall thickening and inflammation. Rectal cultures were negative for N. Gonorrhea, C. Trachomatis, and HSV1/2. LGV complement fixation titers IgG 1:64 and IgA 1:32 indicated prior chlamydia infection. Flexible sigmoidoscopy illuminated erythematous, friable, and ulcerated mucosa in the distal rectum. Histology revealed inflammatory cell infiltration and ulcerations with acute on chronic inflammation. Immunohistochemical staining of rectal biopsy specimens identified spirochetes and reactive RPR was positive with a titer of 1:64, confirming the diagnosis of syphilitic proctitis.
Discussion: The symptoms and endoscopic appearance of infectious proctitis, IBD, and colorectal malignancy overlap. Symptoms can include diarrhea, constipation, dyschezia, hematochezia, tenesmus, and purulent rectal discharge. Endoscopically indistinguishable diffuse rectal inflammation, mucosal thickening, erythema, friable erosions, and ulcerations can be seen. Serological testing and endoscopic biopsy can establish the diagnosis of malignancy, infectious or inflammatory proctitis. The differential for infectious proctitis includes perianal abscess/fistula and in MSM, consider STI’s including gonorrhea, chlamydia, LGV, HSV, syphilis and mpox. Consider HSV or LGV if perianal or mucosal ulcerations are noted. Anogenital HPV infection may manifest as anal warts or anal cancer. Presence of an anal fissure may indicate IBD. Evaluate with anal swabs for STI identification, serology for syphilis and LGV, immunohistochemical staining for syphilis and anal pap for cytology as well as direct endoscopic evaluation and biopsy. Syphilitic proctitis has increased in the past few decades, particularly among MSM. A global systematic review discovered 7 million new syphilis infections in 2020. The prevalence among MSM was 7.5% during 2000-2020 compared to the estimate of syphilis among men in the general population in 2016, 0.5%.6 With a high index of suspicion, a positive RPR and spirochetes on IHC stain confirm the diagnosis.
Conclusions: Given the rarity of syphilitic proctitis and overlap in presentation with IBD, malignancy, and infectious proctitis, it is imperative clinicians consider this diagnosis. Awareness of this atypical presentation, obtaining a detailed sexual history, and evaluating with serology and IHC stain of tissue sample for spirochetes allows for timely diagnosis and treatment, thereby preventing the transmission and late complications of undiagnosed syphilis.