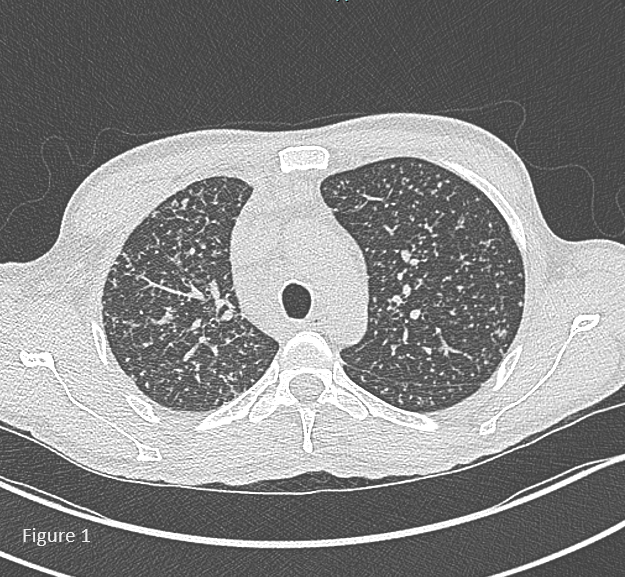
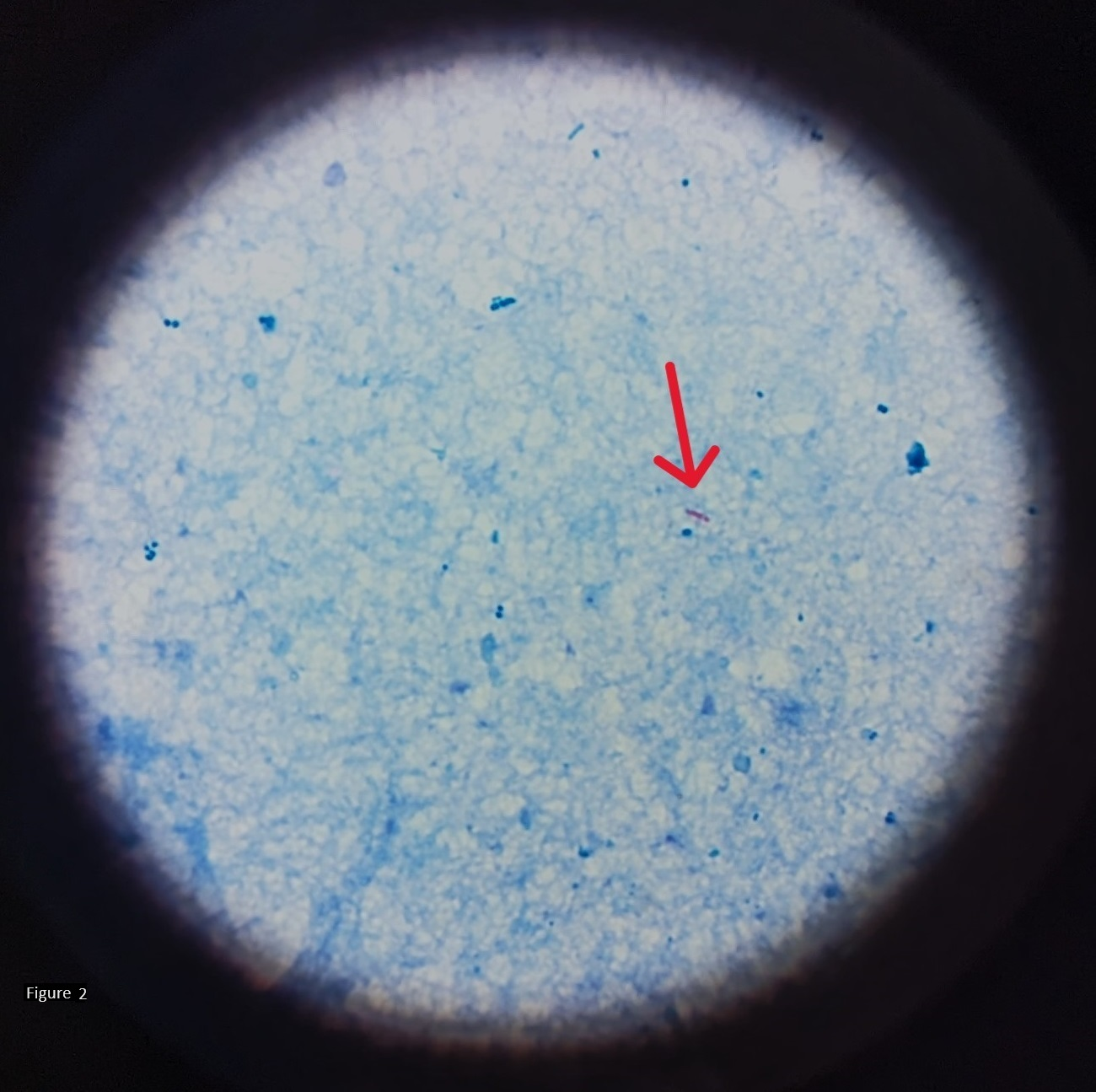
Case Presentation: We detail the hospital course of a 44-year-old man with HIV, inconsistent treatment adherence, and suspected pulmonary tuberculosis (TB). Referred due to miliary lesions on CT scan post-positive QuantiFERON test, weight loss prompted further investigation. The patient, with a CD4 count of 290 cells/μL, had a history of HAART non-adherence, yet no prior AIDS-defining events. Absence of respiratory symptoms, a chest X-ray revealing a suspicious infiltrate, and the inability to expectorate sputum posed diagnostic challenges. Empiric antibiotics were initiated, and stool samples were collected for acid-fast bacilli (AFB) smears before resorting to invasive procedures.Despite initial challenges, pulmonary TB diagnosis was confirmed via high-resolution CT and positive AFB smears from stool samples, prompting appropriate treatment. Due to the patient’s HIV history, Pneumocystis prophylaxis (Mepron/Atovaquone) was initiated, and HAART initiation was delayed due to concerns about immune reconstitution syndrome and potential drug interactions.Multidisciplinary collaboration among Pulmonology, Infectious Disease, and Internal Medicine teams was vital for monitoring and managing the patient’s progress, addressing complications, and preparing for discharge. Outpatient care instructions emphasized directly observed therapy for TB and HIV clinic follow-up.This case underscores the importance of stool sampling for early TB diagnosis, particularly in sputum-inaccessible patients, avoiding prolonged exposure during invasive procedures.
Discussion: While TB is considered controlled in the U.S., latent TB cases pose a risk. Globally, TB remains a leading infectious cause of death, surpassed only by COVID-19 (1). Mycobacterium tuberculosis diagnosis relies on sputum, presenting challenges in non-sputum-producing patients (2).The use of stool specimens as an alternative method for detecting M. tuberculosis organisms has been explored. The idea is based on the survival of M. tuberculosis DNA in swallowed sputum, which may pass through the gastrointestinal tract and be detectable in stool samples. Molecular techniques like PCR show promise in diagnosing pulmonary TB, with studies, including El Khechine et al., demonstrating stool specimens’ potential (3). Their non-invasiveness contrasts with uncomfortable and potentially harmful invasive respiratory procedures.Successful stool culture in developing countries highlights practicality, especially in resource-constrained settings. For HIV patients with smear-negative and extrapulmonary TB, stool cultures offer a valuable diagnostic alternative.
Conclusions: Stool specimens show promise as a non-invasive TB diagnostic alternative, particularly in challenging cases. Further research is vital to establish reliability and applicability across diverse populations. Enhanced diagnostic accuracy promises early TB detection and treatment, reducing public health impact, especially in high-burden regions.