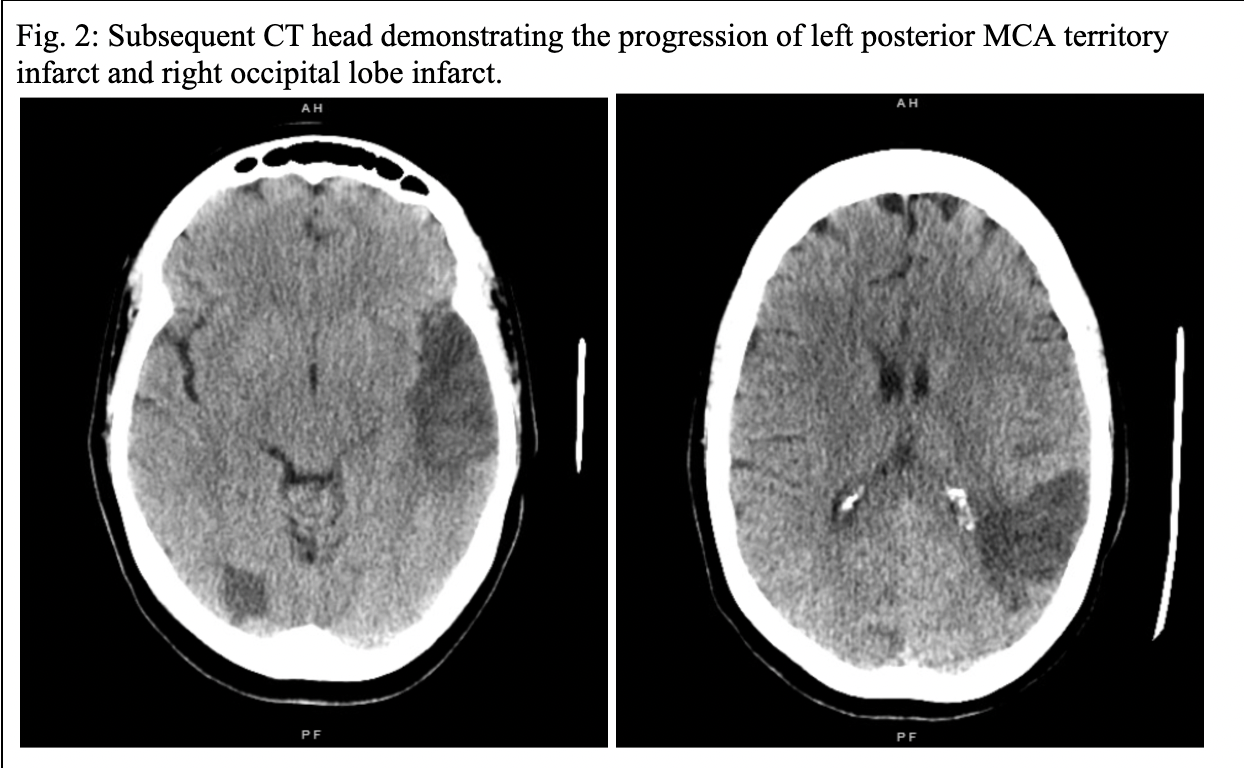
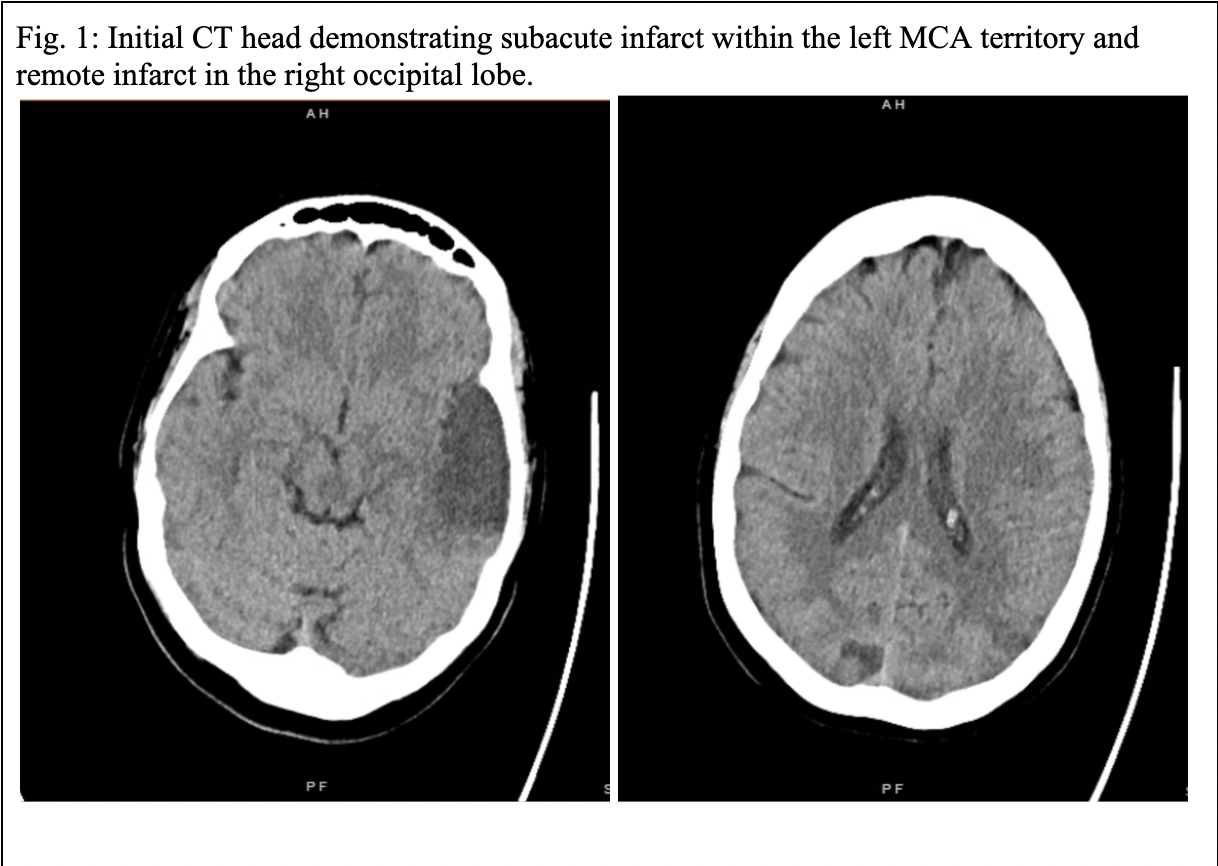
Case Presentation: A 55-year-old female with a past medical history of seizure disorder and prior opioid use presented to an outside emergency department with a 1-day history of expressive aphasia and headache. Her NIH Stroke Scale was 4. CT head w/o contrast demonstrated a subacute infarct within the left middle cerebral artery (MCA) territory and a remote small territory infarct in the right occipital lobe. The patient was loaded with aspirin, refused further work-up and management, and left against medical advice. Of note, the patient was found to have a platelet count of 26 K/uL (140-440 K/uL) during that ED encounter. The patient presented to the hospital 2 days later with worsening aphasia and new-onset blurry vision. Repeat CT head w/o contrast demonstrated progression of bilateral cerebral infarcts, acute infarct in the left parietal lobe, and new cortical infarct in the right occipital lobe lateral to age-indeterminate occipital lobe infarct. Labs demonstrated thrombocytopenia with platelets 27 K/uL (144-440 K/uL), an elevated LDH 970 U/L (98-192 U/L), and low haptoglobin < 10 mg/dL (30-200 mg/dL). No evidence of arrhythmias was noted on electrocardiograms. Transthoracic echocardiogram showed no evidence of wall motion abnormality or thrombus. Blood smears demonstrated the presence of schistocytes with mild to moderate anemia and significant thrombocytopenia. The patient subsequently underwent therapeutic plasma exchange for suspected TTP and was started on oral glucocorticoids with an improvement in platelet count. Her lab results later showed an elevated ADAMTS13 inhibitor at 1.2 BEU (< 0.4 BEU) and decreased ADAMTS13 activity of < 0.03 IU/mL (0.68-1.63 IU/mL) confirming the diagnosis of acquired TTP. Over the course of her hospitalization, bilateral blurry vision and expressive aphasia persisted, and no other focal neurological deficits developed. On discharge, her platelet count was 342 K/uL and LDH was 292 U/L. The patient was discharged home with outpatient follow-up with ophthalmology, hematology/oncology, and nephrology. Unfortunately, 1 week after discharge the patient presented to an outside ED with worsening neurologic deficits and platelet count 4 K/uL confirming relapsing TTP. She suffered cardiac arrest while in the ED and resuscitation efforts were unsuccessful.
Discussion: Thrombotic thrombocytopenic purpura (TTP) is a hematologic disease that can result in hemolytic anemia, thrombocytopenia, and microvascular occlusion secondary to congenital or acquired decreased activity of ADAMTS13[1]. Our case report, in conjunction with prior reports, demonstrates the necessary consideration of TTP for any patient presenting with multifocal ischemic stroke with concurrent thrombocytopenia or anemia. TTP is a hematologic emergency with a 90% mortality rate without treatment, that rate is significantly reduced to 10% to 20% with proper medical management [1, 5]. Particular attention should be noted to any worsening neurological findings during hospitalizations and should be investigated immediately as it may indicate newly developing strokes, as was demonstrated in our patient. The treatment of TTP includes a combination of therapeutic plasma exchange and oral glucocorticoids during acute episodes of thrombocytopenia with conditional recommendations of rituximab and caplacizumab depending on prognostic factors [6].
Conclusions: The importance of considering TTP for any patient presenting with multifocal ischemic stroke with concurrent thrombocytopenia or anemia.