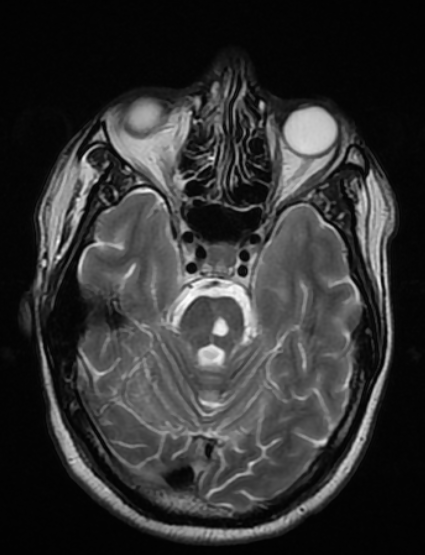
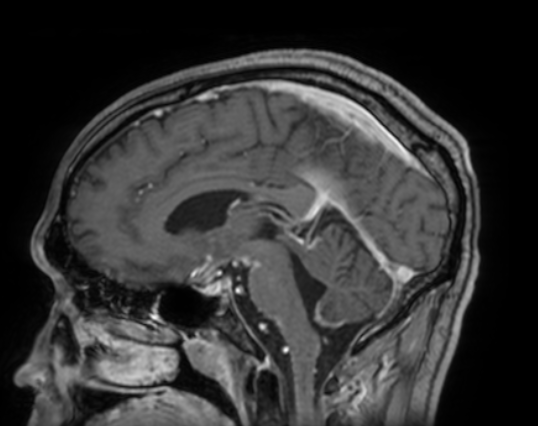
Case Presentation: A 40-year-old man with untreated HIV presented with two weeks of worsening nausea, headache and diplopia. In addition, the patient had some confusion limiting his ability to recall pertinent medical history other than several years ago he was treated for a fungal brain infection. He denied any fevers, weight changes, abdominal pain, or respiratory symptoms. He was unable to adduct his right eye, consistent with a cranial nerve III palsy. MRI was obtained that revealed focal ischemia within the posterior midbrain, within the occulomotor nerve complex, as well as diffuse leptomeningeal enhancement. Initial cerebrospinal fluid (CSF) analysis revealed 285 WBC per ml (81% lymphocytes) and 923 mg/dl protein. RPR was 1:1024. CSF PCR did not detect evidence of bacterial, viral or cryptococcus infection. The patient was started on IV penicillin G for treatment of neurosyphilis, but his symptoms persisted. After obtaining additional medical records, it was discovered that two years prior the patient had been incompletely treated for CNS histoplasmosis. Additional CSF, serum, and urine studies were obtained which revealed similar CSF cell counts of 139 WBC per ml (87% lymphocytes) 760 mg/dl of protein, CSF VDRL ratio of 1:16, CSF FTS-ABS positive, and CSF Histoplasma yeast antibody 1:64. Histoplasma antigen was positive in the CSF, urine, and serum. Treatment with liposomal amphotericin B was immediately started for CNS histoplasmosis. After two weeks of treatment the patient had interval improvement in his nausea and headache.
Discussion: The diagnosis and treatment of CNS infections in HIV patients can prove challenging, especially when provided limited historical information. This case represents the first instance of combined neurosyphilis and CNS histoplasmosis. It was hypothesized that the isolated neurologic symptoms attributed to histoplasmosis were due to incomplete treatment in the past as amphotericin penetration into the CNS is poor. The patient’s other systemic reservoirs may have been eradicated or become latent during his prior partial treatment. Isolated cranial nerve deficits are rare in neurosyphilis but can occur in the meningovascular stage in which infection causes vasculitis resulting in ischemia.(1) CNS histoplasmosis indicates a very poor prognosis. Focal deficits have been seen in up to 30% of patients with CNS histoplasmosis but focal infarction is rare.(2) Both neurosyphilis and CNS histoplasmosis can have leptomeningeal enhancement on MRI as well as CSF lymphocytic pleocytosis with elevated protein. The CSF VDRL test is specific for neurosyphilis but is not very sensitive while CSF FTA-ABS is sensitive but not specific.(1) Serial CSF cell counts after initiating treatment for neurosyphilis can be informative as they should show a response to treatment. CNS histoplasmosis is most commonly diagnosed with CSF antigen and antibody testing.(2)
Conclusions: Despite the availability of advanced diagnostics, this case demonstrates that access to a complete history is of crucial importance. It also demonstrates that even when confronted with a rare and atypical presentation, a thorough evaluation should be made, especially when the patient is not responsive to initial treatment.