Background: The Institute of Medicine includes patient-centeredness as an essential component of high-quality patient care. One dimension of patient-centeredness is the need for physicians to provide clear communication to patients (1). The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey also measures physician communication skill.Patient perception of physician communication is complex. Visual aids such as physician facecards and whiteboards increase the hospitalized patient’s ability to recall their physician’s name (2). Patient satisfaction with physician communication also improves with whiteboard use (3).At our institution, hospitalists have facecards (which include a professional photo, description of role, and contact information) and each patient room has a whiteboard. However, both tools are utilized inconsistently. We designed a project to observe the use and to understand the impact of three communication tools: facecard, whiteboard, and to-do list. We hypothesize that the use of standard communication tools will positively impact patient perception of physician communication in our large and diverse physician group.
Methods: Our study ran from March to May 2022. The participants included a sample of adult patients admitted to medical-surgical units staffed by non-teaching hospitalists. A member of the Patient Experience Team interviewed the patients within 24-48 hours of admission. They asked if: (1) the patient received a physician facecard, (2) the physician used the whiteboard, and (3) the physician used a to-do list. Responses were coded “yes” or “no”. Next, the patient answered three comprehension questions: (1) How well do you understand why you are in the hospital, (2) How well do you understand what steps need to be completed before you leave, and (3) How would you rate the communication skills of the physician? These were answered using a five-point Likert scale with scores 1-3 representing perceived low communication skill and 4-5 representing high communication skill. We used logistic regression analytic models to understand which communication tools yielded higher patient perception scores.
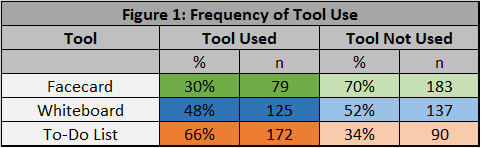
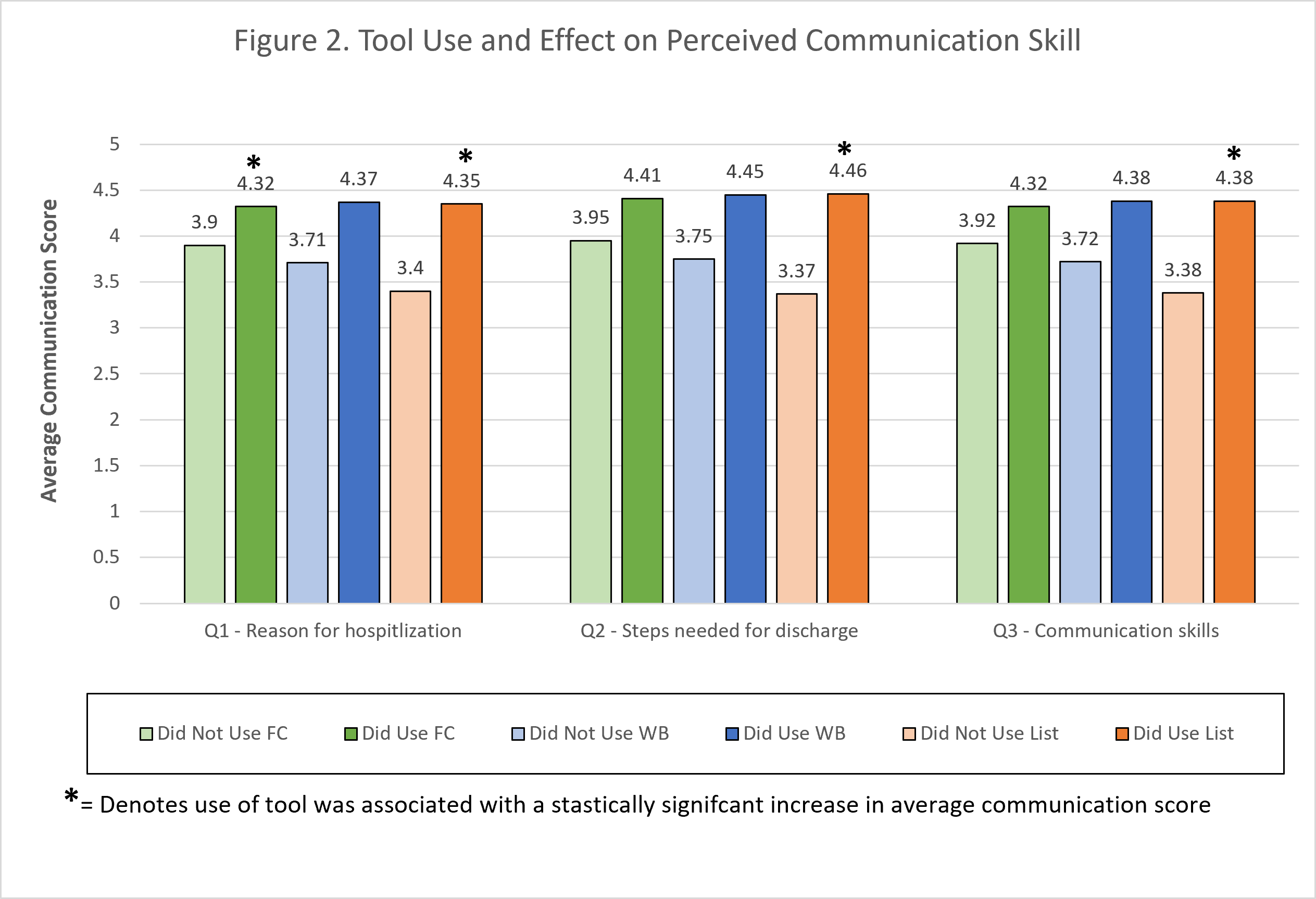
Results: The analyzed sample included 262 patients. The utilization frequency of each communication tool is represented in Figure 1. The perceived physician communication skill was higher for each question group when a tool was utilized (Figure 2). For Question 1, using the facecard and to-do list achieved statistical significance. Facecard use was 2.6 times more likely to receive a high communication skill score. Those who used a to-do list were 21.9 times more likely to receive a high score. On Question 2, the to-do list achieved statistical significance. Those who used the to-do list were 45 times more likely to earn a high score. Also for Question 3, the to-do list returned significance. Those who used the to-do list were over 25 times more likely to earn a high score.
Conclusions: Our results show that not only do communication tools have a positive impact on the patient perception of their physician’s communication skill, but particularly, the use of a to-do list provides the most significant improvement compared to the other tools alone. These results provide a foundation for future projects to standardize the use of communication tools across our large and diverse hospitalist group. Future project goals include: improving communication, increasing HCAHPS physician communication scores, and ultimately providing high quality patient care.