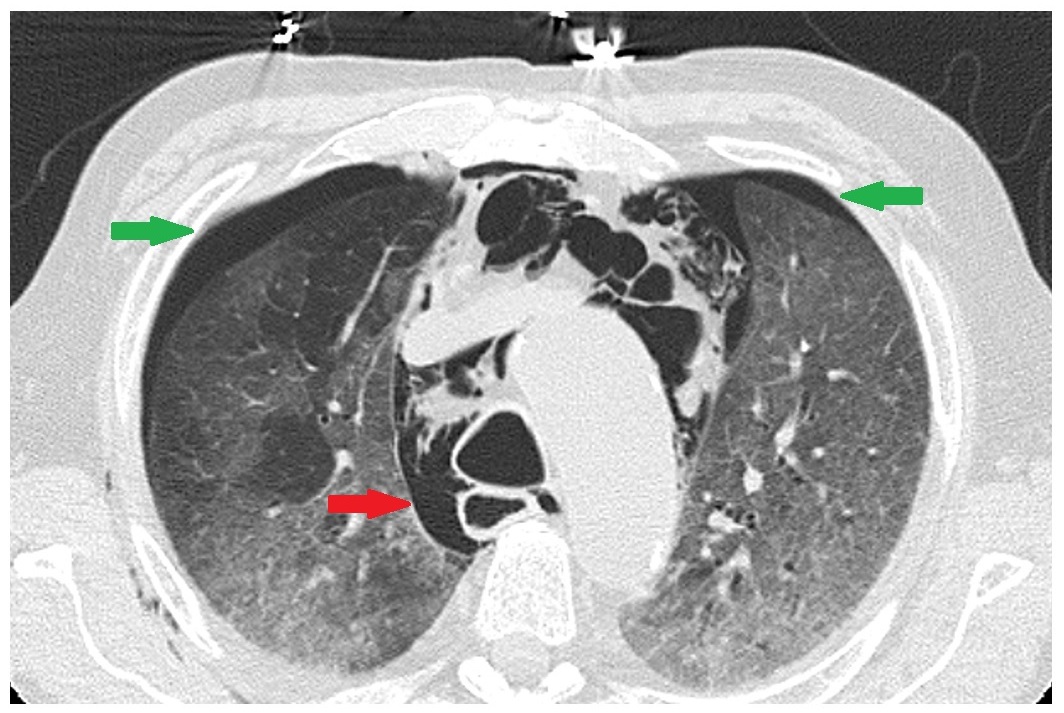
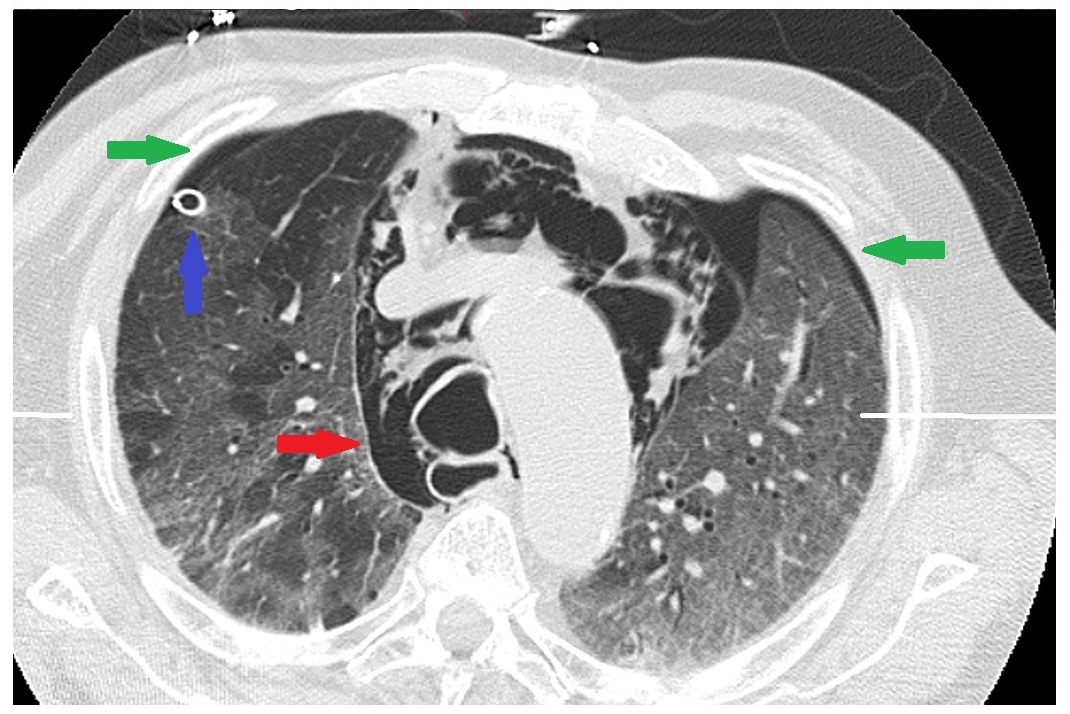
Case Presentation: A 70-year-old male with history of coronary artery disease, paroxysmal atrial flutter, hypertension, prostate cancer presented to the ED due to purulent discharge from his penis and was found incidentally to have COVID-19 on nasal swab. He was started on vancomycin, cefepime, and fluconazole for complicated penile cellulitis. For COVID-19 he was started on dexamethasone and remdesivir. During hospitalization he had progressively worsening acute hypoxic respiratory failure from COVID-19 pneumonia, which required initiation of high-flow nasal cannula and upgrade of care to the Intermediate Care floor (IMC). On day 8 of hospitalization, due to inability to liberate from high-flow nasal cannula, a chest xray was performed which was concerning for pneumomediastinum. A follow up CT scan revealed large bilateral pneumothoraces and pneumomediastinum. He was admitted to the Medical ICU (MICU) where he underwent right sided chest tube placement. The one-sided chest tube improved the bilateral pneumothoraces as well as the pneumomediastinum. Goals of care were discussed, and the patient wished to be DNR/DNI. He was downgraded to the IMC, however, he had worsening respiratory distress and unfortunately passed away from COVID-19.
Discussion: Secondary spontaneous Pneumothorax is emerging as an uncommon complication of severe COVID 19 infections. It is associated with a high morbidity and mortality. One study found an overall in-hospital mortality of secondary spontaneous pneumothorax of any cause to be 4.6%. (1) The mortality appears to be much higher in COVID-19 patients with one case series reporting a 28 day survival of 63.1% (2). The clinical presentation, which includes tachycardia, hypoxia, tachypnea, and shock (3), mimic the presentation of other more common complications of COVID-19 such as superimposed bacterial pneumonia (4), sepsis, and pulmonary embolism (5). As it may present later into the hospitalization, it may be missed on initial imaging. Diagnosis and treatment of pneumothorax must be rapid via a STAT portable chest x-ray and chest tube placement, respectively to minimize morbidity and mortality (3). Compared to other cases of pneumothorax in setting of COVID-19 infection, our case is unique due to the presence of bilateral pneumothoraxes with pneumomediastinum and clinical improvement with placement of a single chest tube. One study found that only 1.3% of inpatient secondary spontaneous pneumothoraxes were bilateral (1). Another retrospective case series of COVID-19 patients who developed pneumothoraxes found that only 2 out of the 60 patients had bilateral pneumothoraxes (2). Hospitalists, being the backbone of inpatient non-ICU management of COVID-19 patients, are in an excellent position to pick up on this.
Conclusions: Pneumothorax is emerging as an uncommon complication of severe COVID-19 infection in hospitalized patients. We highlight the importance of including pneumothorax in the differential diagnosis of severe COVID-19 infections with worsening hypoxic respiratory failure alongside pulmonary embolism, sepsis, and hospital acquired pneumonia. All these complications can present very similarly with hypoxia, tachycardia, chest pain, and shock. The timely diagnosis and management will reduce COVID-19 associated morbidity and, especially, mortality.