Background: Clearly documented patient preferences for treatment at the end-of-life may help inform clinical decision-making during future hospitalizations. The electronic health record (EHR) could facilitate easier access to this information. However, little is known about current documentation practices regarding advanced care planning in the EHR. The objective of this study was to determine the prevalence and content of advanced care planning documentation in the EHR (Epic 2012®) of a single academic teaching hospital, and then to develop a set of local recommendations for best practices.
Methods: We identified all patients discharged from the Hospital Medicine service from January 1, 2015 through October 31, 2015. Using validated automated queries, we collected data on the presence of Physician Orders for Life Sustaining Treatment (POLSTs), a commonly recommended form that documents patients’ wishes for life-sustaining medical treatment and communicates them by creating portable medical orders. We then identified key physician, nurse, social worker and practice manager stakeholders in Palliative Care, Primary Care, Hospital Medicine, Geriatrics, Oncology, and Symptom Management. Stakeholders helped determine a set of best practices for EHR documentation of advanced care planning.
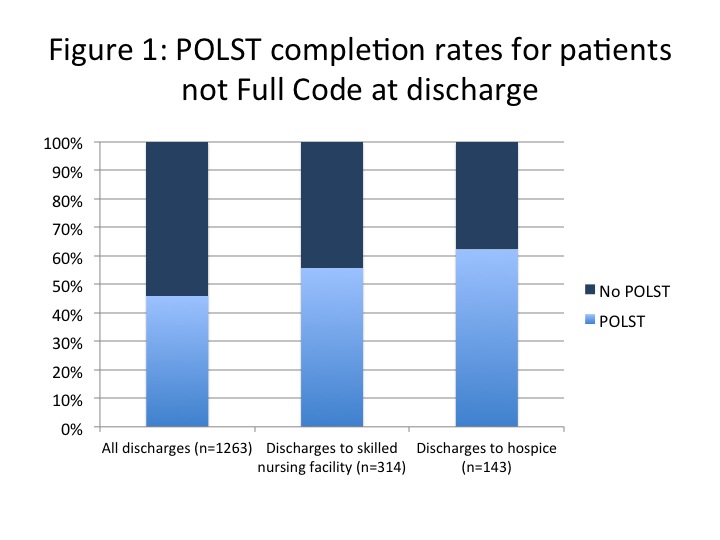
Results: Of the 5671 patients discharged, 1263 (22%) had orders to limit life-sustaining interventions (“Do Not Resuscitate/Do Not Intubate” or “Partial” code orders) at the time of discharge. These preferences were documented in the “Problem List” of the EHR in 1012 (80%) of patients with limits on life-sustaining treatment, and in the discharge summary “Expressed Wishes” section in 1063 (84%) of these patients. POLST forms were not universally completed, even for patients discharged to skilled nursing facilities or hospices (Figure 1).
Our stakeholders identified several key recommendations: a centralized location for advanced care planning documentation in the EHR available to clinicians of all disciplines, improved note templates to assist in standardizing documentation of goals of care, and consistent and highly visible locations in the EHR to display patient surrogate information, POLSTs and advanced directives, and code status.
Conclusions: We found significant room for improvement in documenting patient end-of-life wishes in our EHR, and identified a set of actionable strategies to improve accessibility of advanced care documentation.