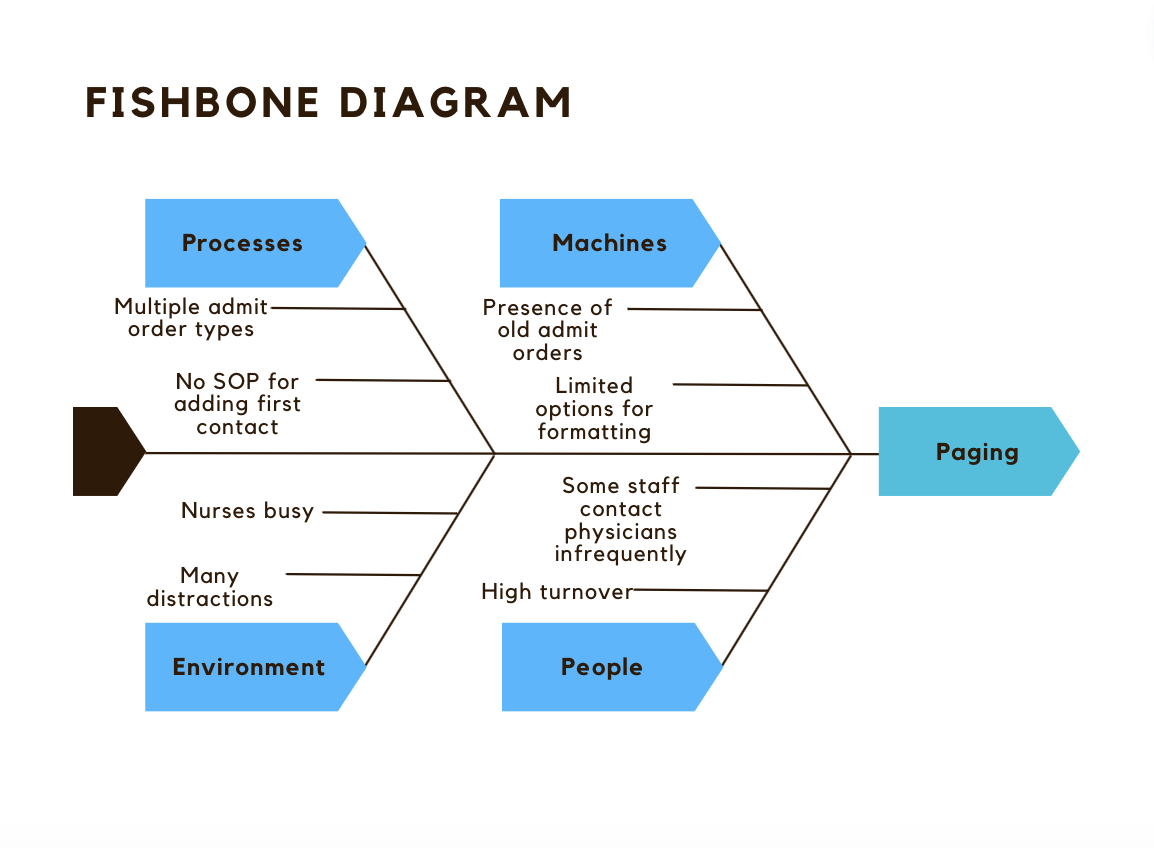
Background: Communication between team members is fundamental to providing high quality care to hospitalized patients (1). Breakdowns in communication lead to compromised patient safety, delays in care, and poor utilization of resources (2). Our Veterans Affairs (VA) hospital has about 200 inpatient beds, primarily staffed by resident physician teams. Bedside nurses use the admission order to identify the physician to page with questions or concerns, referred to as the physician first contact. We have had multiple near miss events when bedside nurses were not able to identify the physician first contact. By investigating these events we learned the direct admission and outside hospital transfer admission orders do not contain physician pagers numbers, and patients admitted through the Emergency Department (ED) that have transferred between teams during their stay have pager numbers in the admission order that are no longer correct. Through a gemba walk we saw the persistence of ED admission orders from prior admissions leads to pager numbers of teams who have previously cared for the patient being displayed in the chart. This results in pages directed to the wrong physician team causing delays in care. The inability to reliably identify the physician first contact was not unique to bedside nurses on the floor. ICU nurses caring for floor patients housed in the ICU and laboratory staff also reported near miss events related to this issue (Figure 1).
Purpose: Our goal is to eliminate pages sent to the wrong physician team. To do this we are implementing multiple interventions to improve identification of the physician first contact. Physicians report pages they receive regarding patients not under their care in a VA secure Microsoft Teams chat to communicate the page to physicians who may be responsible for the patient. We are tracking this data as an outcome measure.
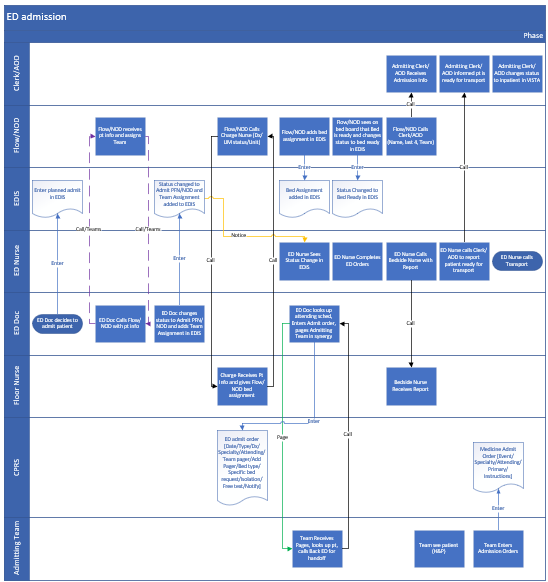
Description: We formed a multidisciplinary team including nurses, physicians, informatics, and the business office. We removed pager numbers from the ED admission order and are creating a new order for entering name and pager number for the physician first contact. This order had to meet the following requirements: be easily visible, be intuitive to identify, have a standard process for entering the order for all types of admissions (ED, direct, and outside hospital transfer), may be edited during the stay, and is deleted upon discharge. We focused on human factors design principles of consistency, signal hierarchy, noise reduction, and attentional capacity. We walked through a process map of each admission type to ensure the new order allowed all parties to have the correct information when they needed it (Figure 2). This group is working to resolve the issue of accumulated admission orders from prior admissions.
Conclusions: Clarifying the physician first contact in the chart required the participation of a multidisciplinary team. The admission orders were not built to identify the physician first contact but were used for this purpose by many hospital staff. As a result, changing the system for identifying the physician first contact required the participation of all parties involved in the admitting process. While meeting the needs of bedside nurses was the impetus for the project, designing a standard, clear, and intuitive solution allowed this system to be used by other groups including ICU nurses and laboratory staff. We are tracking pages directed to the wrong physician team and should have enough data to interpret our statistical process control charts by April 2024.