Background: Urinary tract infections (UTIs) are a common bacterial infection in infants, with potentially serious consequences. Even though urinalysis (UA) is a commonly used screening test for UTI, there is a lack of consensus on its accuracy in well-appearing febrile infants below 28 days old. This study aims to evaluate the accuracy of UA, both alone and in combination with procalcitonin, for detecting UTIs in this age group, with potential implications for managing UTIs in infants.
Methods: This study is a secondary analysis of a retrospective cohort study conducted between 2018 and 2022. The study included well-appearing febrile infants aged 8 to 28 days who presented to the emergency department. Infants were identified for the initial study using the ICD-10 codes for fever, UTI, pyelonephritis, bacteremia, and meningitis. Thereafter, a manual chart review was conducted to ensure that the inclusion criteria were met and to collect additional measures. The study excluded premature infants, those admitted to intensive care units, and those with comorbidities. Infants were eligible for this study if they had a UA evaluating leukocyte esterase (LE), nitrite, and pyuria performed and urine cultures obtained via urethral catheterization. The study evaluated both the individual components of the UA and the UA in aggregate. The study defined UTI as the growth of at least 50,000 CFUs/ml of a known urinary pathogen in culture. For the analysis of the aggregate UA, UA was defined as positive if LE, nitrite, or pyuria (>5 white blood cells/HPF) were present. For the secondary objective, procalcitonin of 0.5 ng/ml or higher was considered positive. Statistical measures, including sensitivity and specificity, were calculated with 95% confidence intervals.
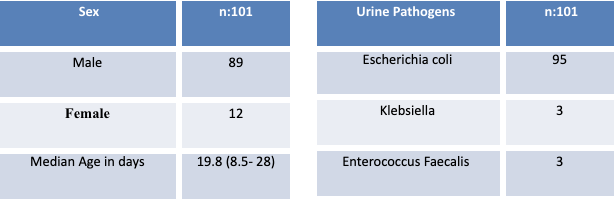
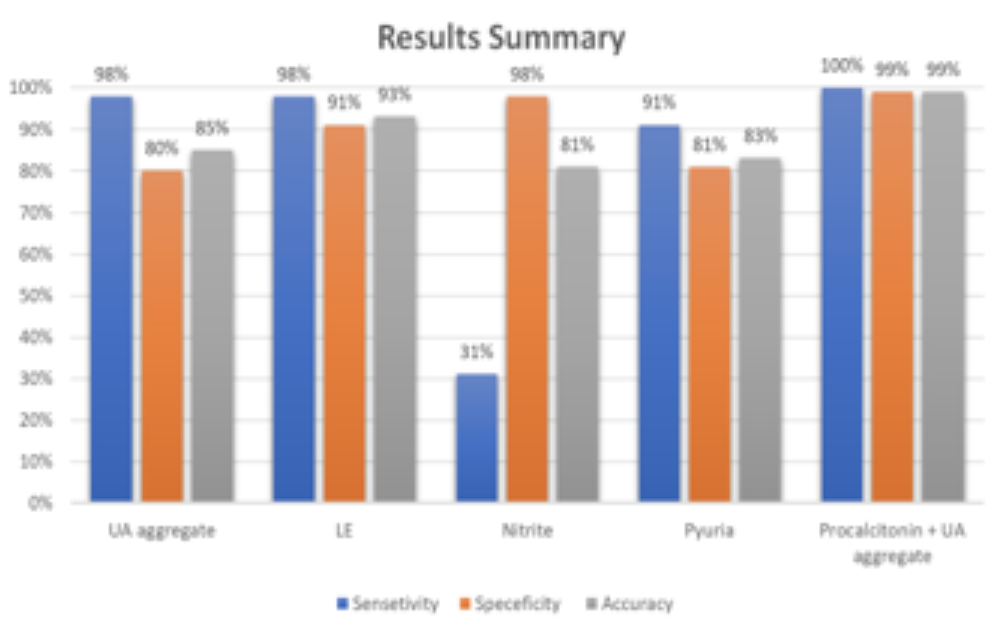
Results: Of 589 infant charts reviewed, 385 met the inclusion criteria, and 101 infants were diagnosed with UTI.The aggregate UA demonstrated a high sensitivity of 0.98 (95%CI:0.93-0.99) and a specificity of 0.80 (95%CI:0.75-0.84). When individual components were evaluated, LE alone showed similar sensitivity for UTI with a higher specificity of 0.91 (95%CI:0.88-0.94), while pyuria demonstrated lower sensitivity and specificity of 0.91 and 0.81 respectively. Nitrite demonstrated the highest specificity of 0.98 (95%CI:0.96–0.99) but a low sensitivity of 0.31 (95%CI:0.22 –0.41). For the secondary objective, there was significant improvement in sensitivity to 1.0 (95%CI:0.9-1.0) and specificity of 0.99 (95% CI:0.94–0.99) when procalcitonin of 0.5 ng/ml or higher was combined with the UA.
Conclusions: Our study presents evidence for potential improvement in precision of UTI diagnosis in febrile infants below 28 days, utilizing a combination of urinalysis and procalcitonin. This approach could potentially enhance the confidence of clinicians in their initial suspicion of UTI while awaiting urine culture results. However, given the limited sample size in this study, further research with a larger cohort is necessary to validate these findings and assess the feasibility of implementing this approach.