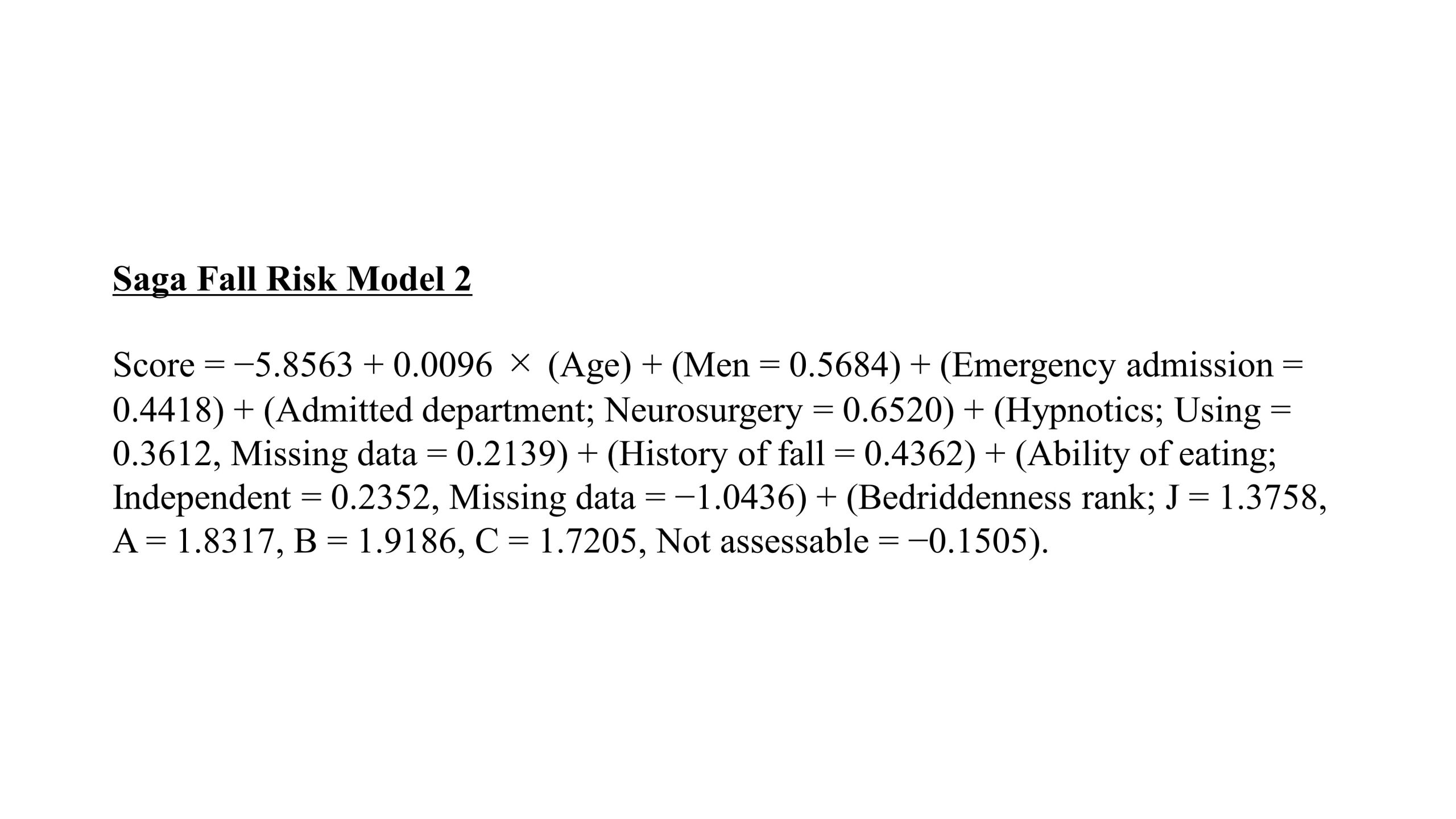
Background: We conducted a pilot study in an acute care hospital and developed the Saga Fall Risk Model 2 (SFRM2), a fall prediction model comprising eight items: Bedriddenness rank, age, sex, emergency admission, admission to the neurosurgery department, history of falls, independence of eating, and use of hypnotics. Bedriddenness rank is an official scale of activity of daily living widely used in healthcare settings in Japan. Hypnotic medications were defined as benzodiazepines and non-benzodiazepines excluding melatonin receptor agonists and orexin receptor antagonists (Figure 1). The external validation results from the two hospitals showed that the area under the curve (AUC) of SFRM2 may be lower in other facilities. This study aimed to validate the accuracy of SFRM2 using data from eight hospitals, including chronic care hospitals, and adjust the coefficients to improve the accuracy of SFRM2 and validate it.
Methods: This is a multicenter retrospective observational study. This study included all patients aged ≥20 years admitted to eight hospitals, including chronic care, acute care, and tertiary hospitals, from April 1, 2018 to March 31, 2021. In-hospital falls were used as the outcome, and individual scores for SFRM2 were calculated for each patient, and the AUC of SFRM2, 95% confidence interval (95% CI), and shrinkage coefficient were determined. Additionally, SFRM2.1, which was modified from the coefficients of SFRM2 using logistic regression with the eight items comprising SFRM2, was developed using two-thirds of the data randomly selected from the entire population, and its accuracy was validated using the remaining one-third portion of the data. For the SFRM2 scores of the entire population and the SFRM2.1 scores of the validation set, we computed fall probabilities, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for cutoff values derived using the Youden index.
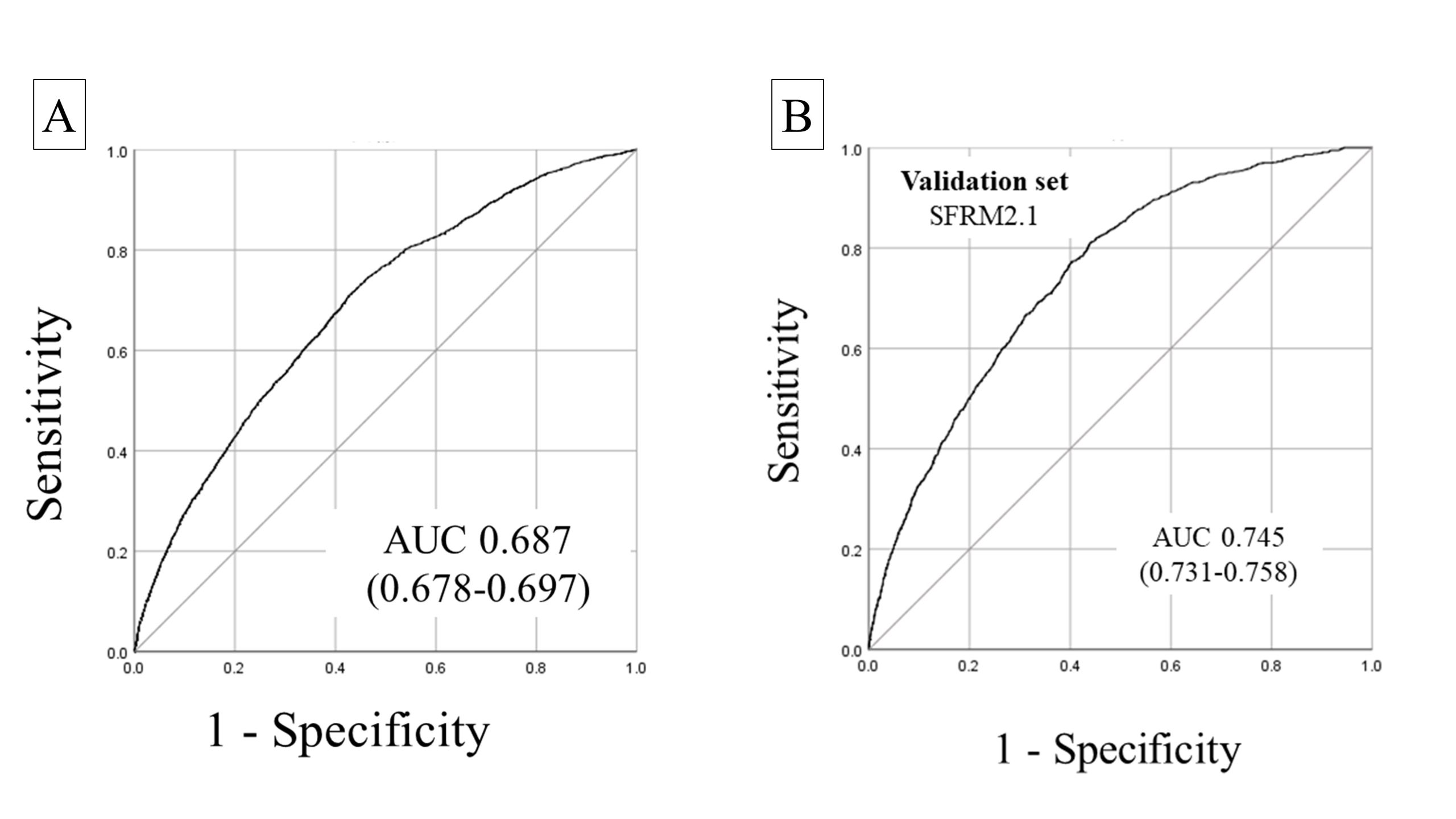
Results: Of the 124,521 inpatients analyzed, 2,986 (2.4%) experienced falls during hospitalization. The median age of all inpatients was 71 years, and 53.2% were men. The AUC of SFRM2 was 0.687 (95% CI:0.678–0.697), and the shrinkage coefficient was 0.996 (Figure 2-A). The cutoff value for the Youden index was − 2.85. The corresponding PPV and NPV values for each cut-off point were 3.9% and 98.8%, respectively. SFRM2.1 was created using 81,790 patients, and its accuracy was validated using the remaining 42,731 patients. The AUC of SFRM2.1 was 0.745 (95% CI: 0.731–0.758) (Figure 2-B). In the validation set, the cutoff value for the Youden index was determined to be − 4.02. The corresponding PPV and NPV values for each cutoff point were 4.4% and 99.2%, respectively.
Conclusions: The SFRM2, which are particularly useful in predicting falls, showed good ability to predict falls in the validation in diverse populations with significant background variations. Furthermore, it is possible to improve the accuracy by adjusting the coefficients while keeping the model parameters fixed. The easy-to-evaluate SFRM2 can lead to accurate prediction of falls among inpatients, thereby enhancing the quality of healthcare safety by efficiently allocating medical resources and preventing falls.