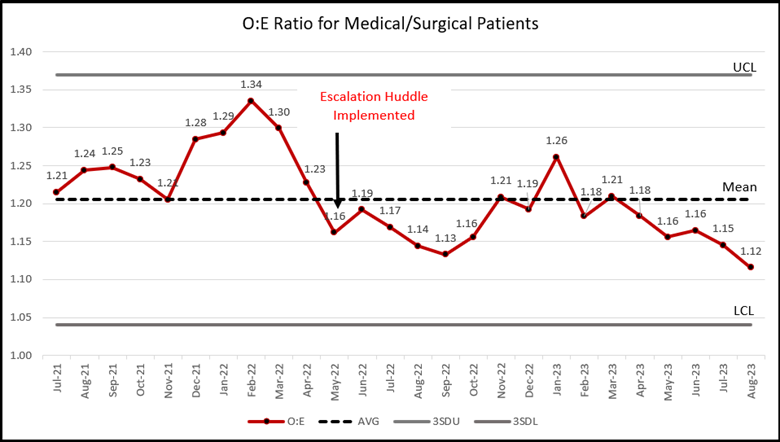
Background: Interdisciplinary Rounds (IDRs) are essential for coordinating patient care on hospital units within the two acute care hospitals of St. Peter’s Health Partners located in Albany, New York (a 440-bed tertiary care hospital and a 160-bed hospital). However, with a length of stay O:E ratio as high as 1.34, we were concerned that not all barriers to patient progression were being addressed timely and that provider clinical practice variability might be contributing to excess hospital days.
Purpose: The study aimed to conduct a daily “Escalation Huddle” across the health system to achieve a reduction in the O:E for length of stay, facilitate cross-departmental communication to reduce systematic barriers to discharge, and better understand provider practice variation.
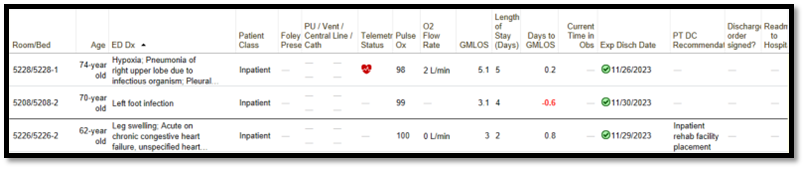
Description: A daily 25-minute virtual huddle facilitated by a Hospitalist team leader convened various departments including therapies, radiology, procedural areas, home visiting nurses, and hospice. Unit-based IDRs continued as they had previously and were performed prior to the 12:30pm Escalation Huddle. Equipped with the information from their unit’s IDRs, nurse managers from each ward presented patients with an expected discharge date of tomorrow and briefly explained “why not today?”. They also escalated any system-based process issues impeding today’s care progression for specific patients.Ancillary departments reprioritized patients to support same-day discharges. Utilizing the Epic dashboard (Figure 1), the Hospitalist facilitator was able to get a high-level overview of each patient. If the reason for discharge tomorrow did not adhere to accepted clinical discharge standards, the Hospitalist facilitator communicated with providers and offered guidance and suggestions.
Conclusions: The Escalation Huddle process ensured better team understanding of patient care plans and clinical standards for discharge. We learned there was significant provider practice variation regarding individual thresholds to discharge. With this information and specific examples, we created objective discharge standards which were reinforced through the daily Escalation Huddle.The practice of waiting for the following day to discharge patients with minor issues was replaced by reevaluation later in the day. This approach emphasized viewing patient stays in hours rather than calendar days. The daily involvement of a Hospitalist leader improved communication between nurse leaders and providers and empowered nurse managers to ask non-confrontational questions to providers during IDRs. The Escalation Huddle process allowed for immediate issue resolution and encouraged real-time problem solving.The improvements in provider clinical practice and real-time barrier resolution led to a reduction in the health system’s O:E ratio from an average of 1.25 the year prior to the intervention to 1.18 in the year following the intervention (Figure 2), with less variability. A daily “Escalation Huddle”, as implemented in this study, successfully improved patient care coordination, reduced clinical practice variability, and resolved patient progression barriers in real-time. These improvements ultimately led to a significant reduction in the O:E ratio for length of stay. This model can serve as a valuable framework for enhancing care progression in acute care hospitals.