Background: Though the ACGME dictates that Internal medicine residents should be exposed to the domains of quality improvement (QI) and medical education (Med Ed), most residency programs provide limited opportunities to develop these skills. Furthermore, most existing hospital medicine electives which attempt to cover these topics are 4 weeks in length.
Purpose: We sought to create a compressed two week hospital medicine elective for internal medicine residents, which includes 7 days in clinical hospital medicine mentorship and dedicates 4 days to personalized, mentored, hands on experience in medical education and quality improvement experiences. To our knowledge, we are the first program to document a meaningful structured practicum in these non-clinical domains which fits into such a compressed timeline.
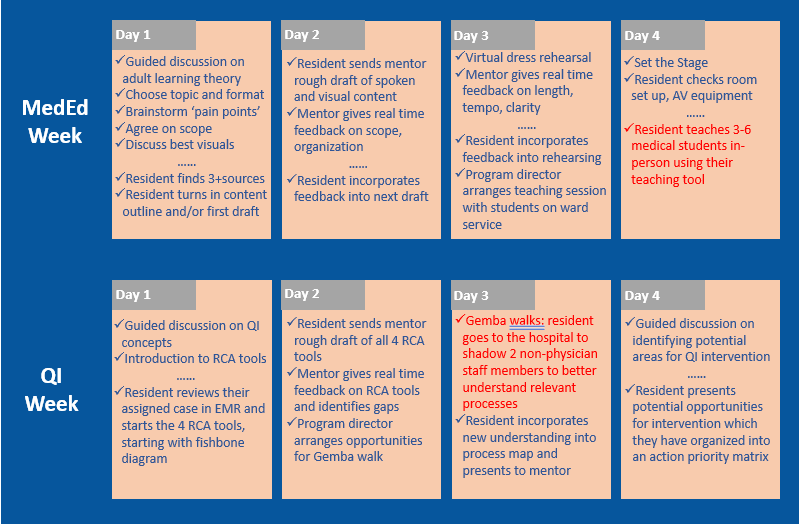
Description: Our curricular improvement initiative was composed of one clinical week and one 4-day non-clinical week where residents choose to complete a quality improvement (QI) or medical education (MedEd) practicum. The residents who choose medical education create a teaching tool through multiple rounds of real-time feedback with the hospital medicine faculty mentor. Over the course of the week, the mentor teaches them about adult learning theory and strategies to augment learners’ attention, such as repetition of key concepts, building an interactive talk, making the topic accessible to various levels of learners, and limiting the length and extent of the material covered and using hooks. The mentor guides the resident in brainstorming their own teaching topic, and choosing an appropriate format. Residents are given the option to learn to use the online visual content creation tool CanvaTM. The mentor gives candid feedback on the scope, organization, and aesthetics of the residents’ content, as well as resident’s teaching style, tempo and clarity of spoken content. At the end of the week, residents use the teaching tool to deliver a didactic to medical students. The residents who choose quality improvement complete a root cause analysis of a real patient case from our hospital. The faculty mentor walks the resident through four tools to perform a root cause analysis (RCA). The resident is then assigned an actual patient case to investigate, which are chosen by our director of patient safety. The resident then goes into the hospital for two “Gemba walks” where they shadow non-physician staff members to assess the environment applicable to their patient case. The resident identifies potential QI interventions and learns how to organize these into an action priority matrix. After the rotation, the resident is given the option to present the case at a resident patient safety conference.
Conclusions: We created a time efficient, two-week curriculum to teach residents skills in quality improvement and medical education. While many 4-week long hospital medicine rotations exist at top internal medicine programs, our elective represents one of the first examples of meaningful QI and MedEd training in such a compressed timeline. Despite its brevity, our elective allows each resident highly personalized and hands-on experience due to our low ratio of residents to faculty, highly structure 4-day practicum, and continuous interactive components. Our HM rotation has been well received by residents and faculty alike.