Background: Multiple safety reports were reviewed for missed doses of critical medications on admission to the inpatient rehabilitation units at a large academic medical center. It was found that providers were inconsistently or incorrectly using the admission medication reconciliation (AdmMedRec) functionality in EHR that could have prevented these errors.Many hospitals struggle with AdmMedRec due to low physician engagement or lack of perceived value1. Successful interventions have used hard-stops or pop-up alerts to prevent or interrupt order entry until AdmMedRec was complete2,3. However, such implementation can be dissatisfying to providers and disruptive to workflow. Designing clinical decision support can also be a time-consuming process that requires consensus building through various levels of governance structure. A hospitalist-clinical informaticist was engaged to review the AdmMedRec process and to design an intervention to improve AdmMedRec completion rate by focusing on 3 key areas: knowledge, process, and culture.
Methods: Existing workflow was assessed to identify knowledge gap. A step-by-step process for completing AdmMedRec was designed to specifically tailor to the workflow of the intervention units and incorporated rarely used EHR tools such as flags and checklists into the provider daily routine to bring visibility of its completion status. A one-hour, interactive, case-based education session covered both the technical knowledge and the cognitive evaluation of different data sources to generate a single prior-to-admission medication list.Visible physician and administrative leadership support were essential to the intervention. AdmMedRec completion was added to the performance metric for the units. The education session was placed on the required didactic schedule for the residents and attended by the department chair. We compared AdmMedRec completion rates pre- and post-intervention and between intervention units and the rest of the hospital (control).
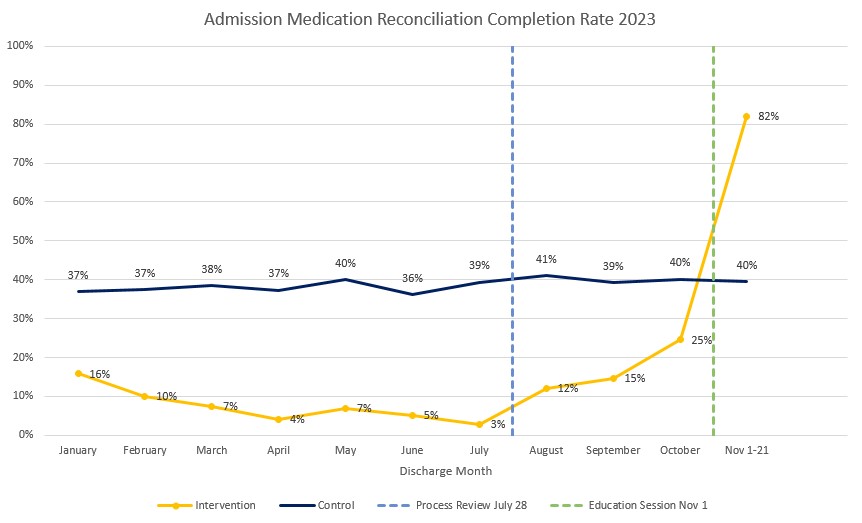
Results: The completion rate for AdmMedRec for patients discharged from the intervention and control units during the prior fiscal year (July-June) were 13% and 38%, respectively. A gradual increase in the completion rate was observed on the intervention units in the 3 months following the initial process review with the provider champion (see chart). In the four weeks immediately after the education session, the completion rate significantly increased to 82% on the intervention units, while it remained unchanged for control.
Conclusions: Preliminary results showed that our intervention was highly successful in increasing AdmMedRec completion rate without the need for an EHR-based interruptive alert or adding resources such as pharmacists. Previous studies have found varying successes through training3. We postulate that our success was due to a curriculum that was tailored to the specific scenarios and challenges frequently encountered by the providers on the intervention units. We believe that all 3 components of the intervention are highly critical to its success. Providers must have the knowledge to perform the cognitive and technical tasks of AdmMedRec, have the visibility to the completion status in real-time, and recognize it as a priority in the organization’s culture of safety. Additional data will be collected to see if the success can be sustained over time, if a high completion rate is associated with a decrease in the number of medication errors, and if a similar approach can be replicated in other units.