Background: Academic hospitalists aspire to be highly effective teachers and must demonstrate excellence in teaching to be promoted. Internal Medicine (IM) residency programs increasingly rely on such hospitalists to supervise residents when they are on inpatient service. Accordingly, outstanding resident teaching and evaluations are imperative to the advancement of academic hospitalists and the success of both Hospital Medicine services and IM residency programs.
Purpose: We sought to coach and mentor academic hospitalists before their first ward teaching rotation with a just-in-time training bundle to optimize the resident learning experience.
Description: The Hospital Medicine Education Committee Chair and the Director of Faculty Development conducted a thorough literature search and met with highly rated clinical teachers across multiple programs at the institution, including the Internal Medicine Residency Program Director, to identify best practices in teaching during inpatient medicine wards, qualities of excellent attendings as well as perceived deficits. Based on this information, a training bundle was developed which included a content rich didactic session, common ward scenarios for discussion, a small group mentoring session with top-rated faculty, information on best practices in adult learning and resources for didactic teaching.
The 90-minute, small group (2-3 senior, 2-3 junior faculty) training takes place 1 week prior to the faculty’s first inpatient medicine ward block. The didactic session contains logistical details, program expectations, teaching pearls on core clinical domains, and best practices in inpatient medicine ward teaching. Ward scenarios incorporate situations on learning climate, clinical teaching, teaching styles, communicating expectations and team management. During the mentoring session, senior faculty provide pearls on how to lead inpatient medicine ward teams, including how to manage a call day, balancing rounding times, autonomy vs. supervision, providing feedback as well as personal anecdotes of successes and failures.
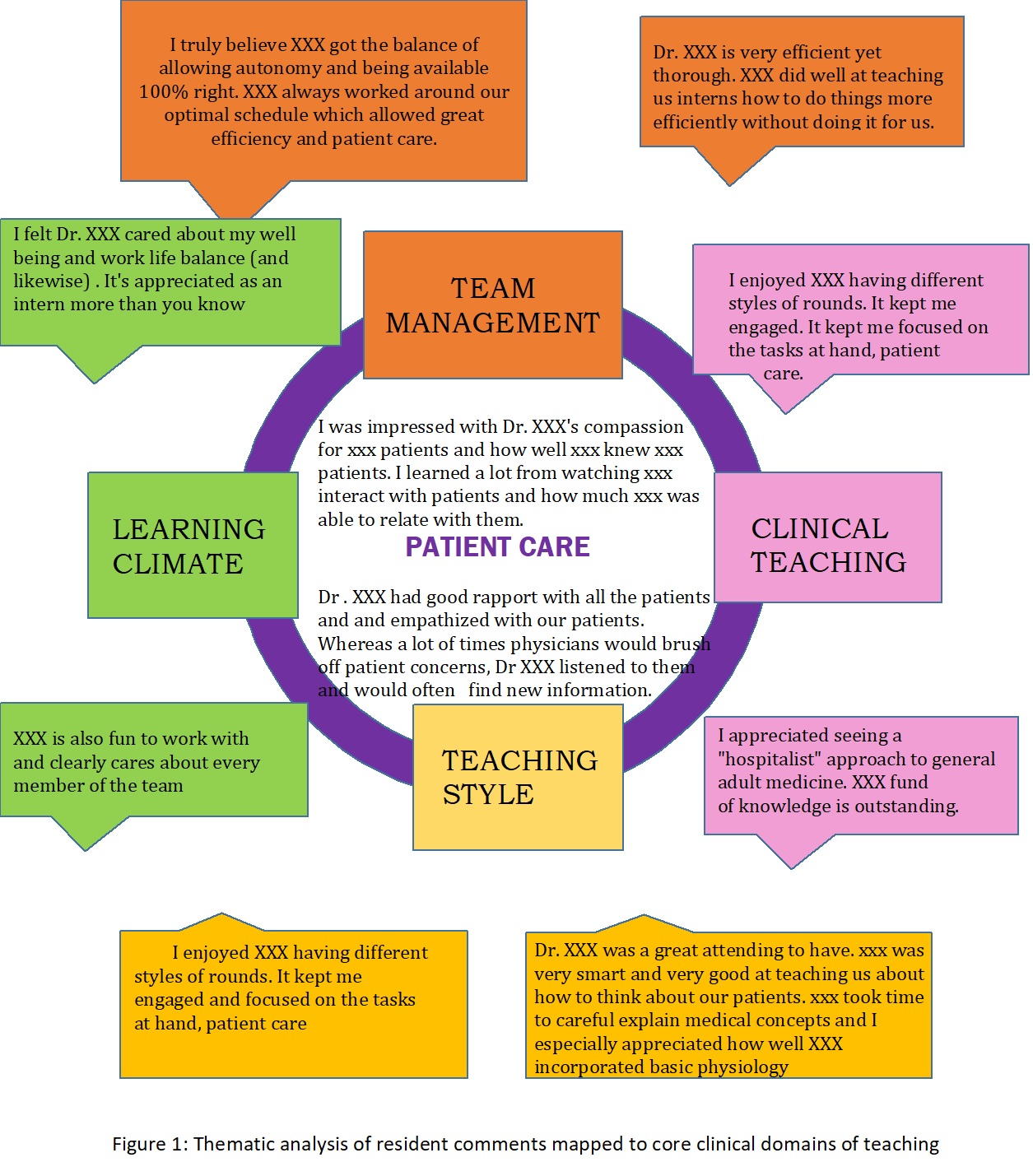
Mirrored, pre- and post-surveys were administered to the new faculty members. Qualitative data was obtained for faculty based on resident comments and analyzed for themes and sub-themes (Figure 1). Quantitative faculty evaluation data will soon be available after it meets confidentiality regulations.
Conclusions: Using institution-wide expert opinions as well as literature on best practices in inpatient medicine ward teaching, we developed a just-in-time training bundle to catalyze the teaching performance of academic hospitalists. This has been well received by the faculty new to inpatient medicine ward teaching and initial feedback suggests that residents also have benefited from the program.