Background: Patients with sickle cell disease (SCD) experience painful and life threatening vaso-occlusive episodes (VOE) that cause frequent hospitalizations, account for >80% of their >$1 million lifetime healthcare costs, and can be fatal. Yet, there is a dearth of evidence addressing inpatient VOE care leading to a stark absence of evidence-informed guidelines. As a first step towards improving inpatient VOE care, we aimed to explore what ideal inpatient VOE care should look like from both the patient and healthcare team perspectives.
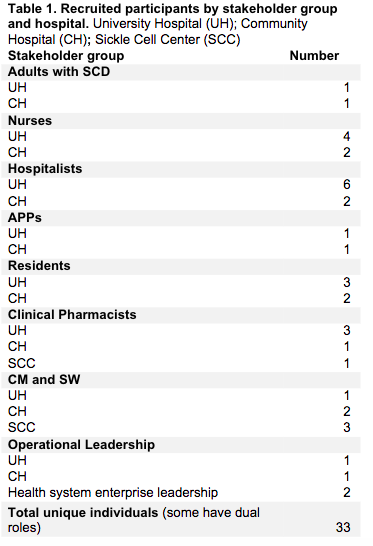
Methods: We conducted a qualitative study using a phenomenological approach from 1/2022 to 11/2023. Using purposive sampling, we recruited adults with SCD and inpatient healthcare team stakeholders at a university-based hospital, a community hospital, and an outpatient sickle cell center (Table 1) to participate in semi-structured interviews and focus groups. Our interview and focus group guides were informed by the Health Equity Implementation Framework and Systems Engineering Initiative for Patient Safety model in order to explore multi-level factors that may impact VOE inpatient care. Prompts included questions for all stakeholders like, “Tell me about your most recent experience (in the hospital for SCD)/(caring for someone with SCD)” and “In an ideal world, what would inpatient VOE care look like?”. Others were specific to a stakeholder group (e.g., “Do you feel equipped to take care of patients with SCD who are in the hospital?” for healthcare team members). Interviews and focus groups were recorded and transcribed, and the data were analyzed using thematic analysis.
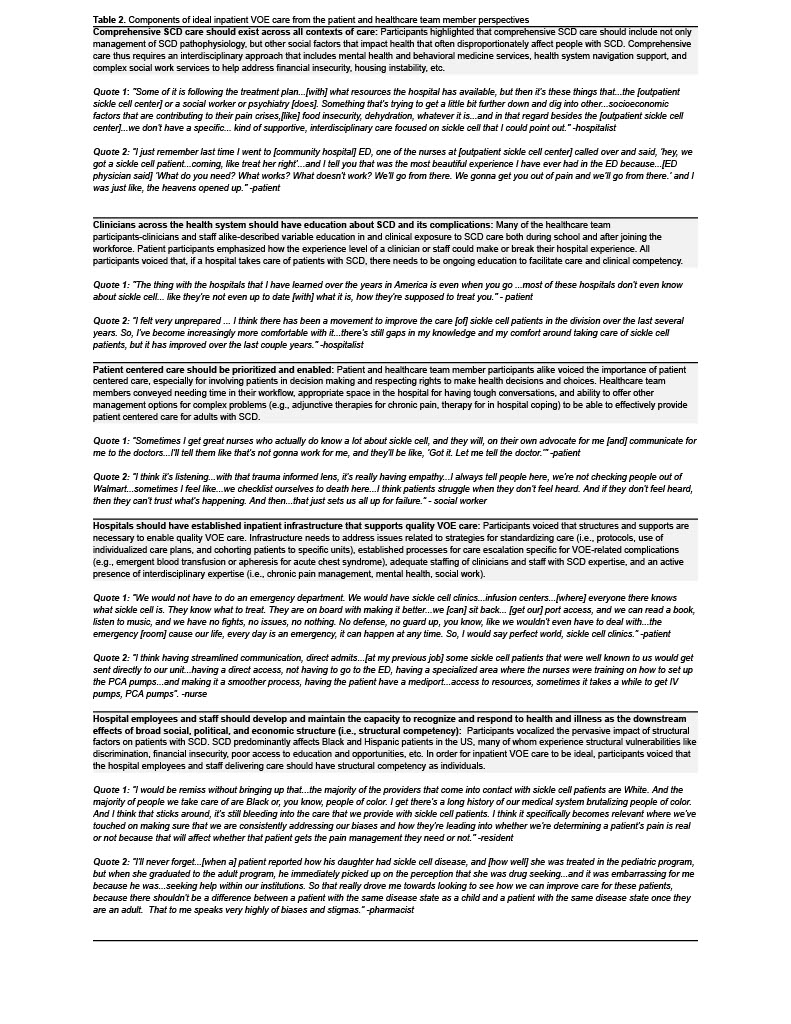
Results: We interviewed and facilitated focus groups with thirty-two participants (Table 1). Participants, regardless of stakeholder group, were consistent in highlighting five key areas that should be a part of ideal inpatient VOE care (Table 2 for description and quotes): 1) Comprehensive SCD care should exist across all contexts of care; 2) Clinicians across the health system should have education about SCD and its complications; 3) Patient centered care should be prioritized and enabled; 4) Hospitals should have established inpatient infrastructure that supports quality VOE care; 5) Hospital employees and staff should develop and maintain the capacity to recognize and respond to health and illness as the downstream effects of broad social, political, and economic structure (i.e., structural competency).
Conclusions: Patients with SCD and healthcare team members described key components of inpatient VOE care, most of which have substantial room for improvement. Implementing these aspects of care requires growth in the evidence base for VOE care as well as investment in system infrastructure. This infrastructure includes establishing comprehensive SCD care, prioritizing education for all healthcare team members regarding SCD and structural competency, and addressing the resource strain in the inpatient care setting that disproportionately affects marginalized patients like those with SCD. While working on these system-level changes, individuals on the healthcare team should lean on and include the expertise of both the interdisciplinary team and the patient as a plan of care is created and adjusted.