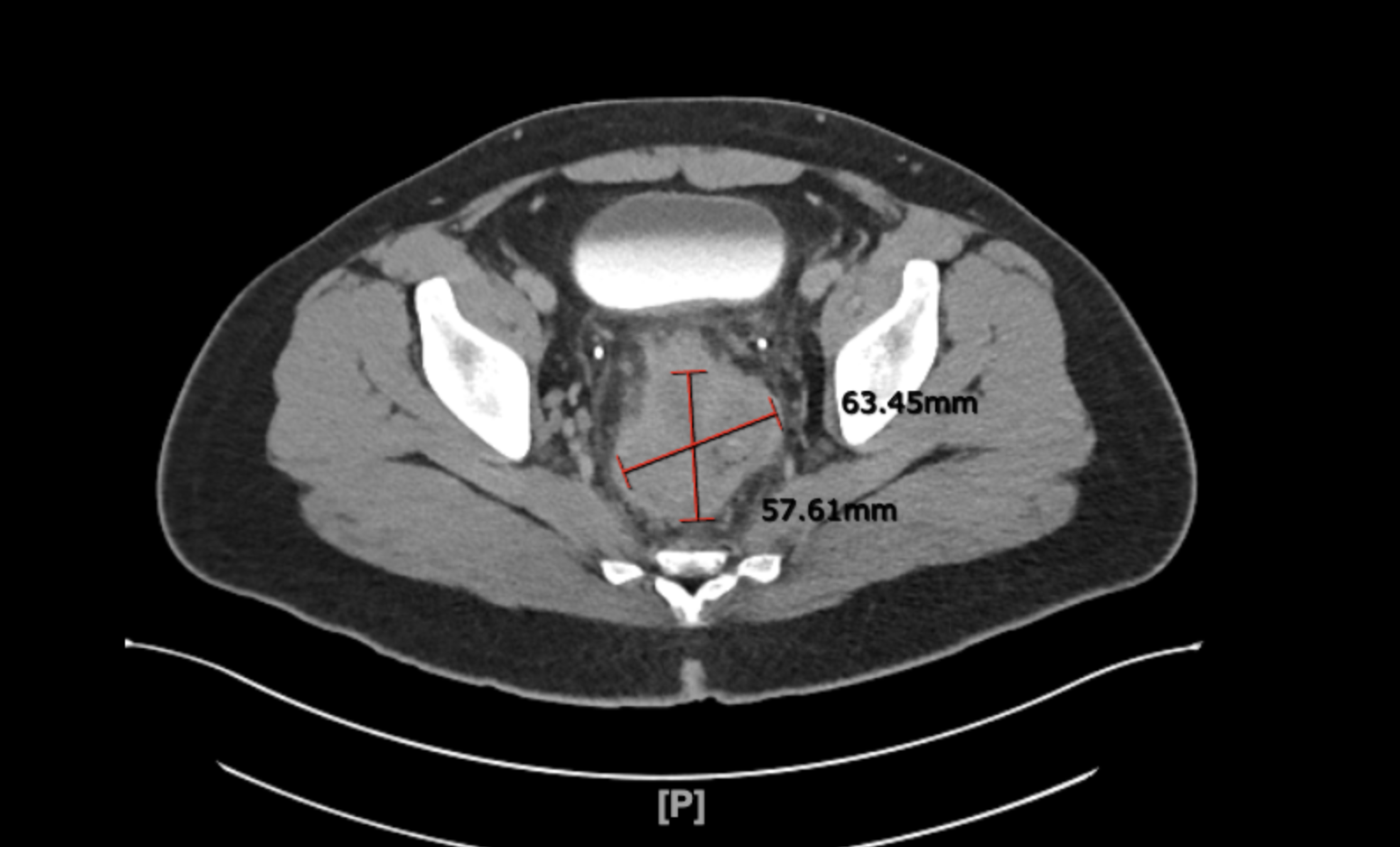
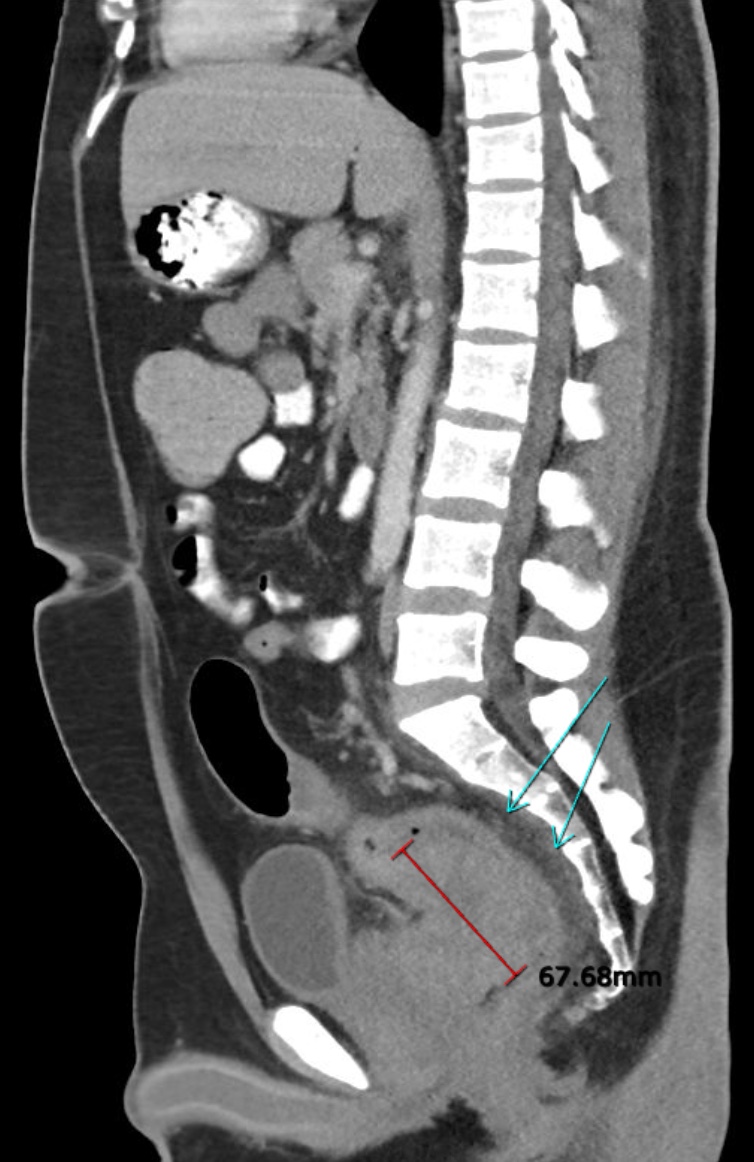
Case Presentation: A 27-year-old man without significant medical history presented with constipation and weight loss of 25 pounds in 2 months. A digital rectal examination revealed a fungating mass in the rectum. CT abdomen/pelvis showed the presence of a large intraluminal rectal mass measuring 6.8 X 5.8 X 6.3 cm with no evidence of metastasis. The family history was significant for colorectal cancer in his father, paternal grandfather, and paternal uncle. Flexible sigmoidoscopy with biopsy showed an invasive adenocarcinoma with MLH1 and PMS2 loss of expression. Based on pelvic MRI findings, Stage III(T4N1) rectal cancer was diagnosed. After a multidisciplinary discussion involving the surgeon, radiation oncologist, and oncologist, the decision was made to proceed with neoadjuvant chemotherapy, concurrent chemoradiation, surgery, and adjuvant chemotherapy. He was treated with neoadjuvant FOLFOX(leucovorin, fluorouracil, and oxaliplatin) for 6 cycles. A pelvic MRI after treatment showed a complete resolution of the initial mass. PET scan showed a small focus of residual active malignancy in the anterior wall of the rectum. Concurrent chemoradiotherapy with capecitabine was done followed by robotic-assisted laparoscopic low anterior resection. The final pathology did not show any residual disease. Adjuvant chemotherapy with XELOX(oxaliplatin and capecitabine) 4 cycles was completed. The follow-up appointments with CT chest/abdomen/pelvis and CEA showed no signs of recurrence. He is instructed to get regular screening with upper endoscopy every 3 years, colonoscopy, urinalysis, and skin examination every year.
Discussion: This case illustrates the full picture of a patient with Lynch syndrome diagnosed with locally advanced rectal cancer. There are several teaching points that this case offers:1) In young patients diagnosed with colorectal cancer, a thorough investigation of family history is required. If there is a positive family history, genetic testing to rule out Lynch syndrome is strongly recommended.2) The strategy for treating rectal cancer in Lynch syndrome is continuously researched. A recently published journal proved that the efficacy of chemotherapy alone in patients with 20% or more response is not inferior to chemoradiation. 3) In another prospective phase 2 study, neoadjuvant immunotherapy with dostarlimab was proven effective for MMR-defective, locally advanced rectal cancer. For the patient’s optimal outcome, updated treatment options should be studied and considered. 4) According to the Centers for Disease Control and Prevention, It is important to instruct patients with Lynch syndrome to undergo the recommended screening of multiple organs appropriate for age. It includes colonoscopy every 1-2 years beginning at age 20-25, EGD every 3-5 years starting at age 40, annual urine analysis and neurologic exam starting at age 25-30. Additionally, for women, endometrial biopsy every 1-2 years is recommended followed by prophylactic hysterectomy and salpingo-oophoroectomy when childbearing is completed.
Conclusions: Lynch syndrome(hereditary non‐polyposis colorectal cancer) is characterized by an increased chance of developing cancer in various organs in the setting of mutation in one of the mismatch repair(MMR) genes: MLH1, MSH2, MSH6, or PMS2. This case report illustrates a patient with MMR-defective rectal cancer who has responded well to the standardized therapy and suggests other possible treatment options with up-to-date research outcomes.