Background: Patient & Family Advisory Councils (PFACs) are groups of patients and caregivers who share their overall experiences of care and perspectives on specific topics with hospital leaders at regular meetings. PFACs provide a crucial supplemental layer of feedback to hospitals outside of HCAHPS survey data and post-discharge phone calls. Hospital Medicine specific PFACs are less common due to a lack of continuity in acute care settings, the heterogeneity of patient backgrounds on an inpatient medicine service, variability in illness types and severity, and physicians’ lack of familiarity with patient engagement strategies.
Purpose: To create and operationalize a Hospital Medicine specific PFAC using previously researched best practice patient engagement methodologies.
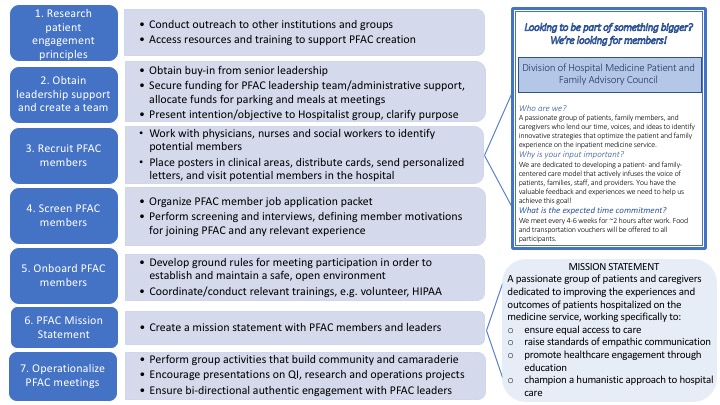
Description: Starting in July 2017 we employed a consultative and collaborative approach to create a Hospital Medicine specific PFAC. To do this, we utilized an iterative process of best practice tools and methodologies for patient engagement we had researched previously (Figure 1). We obtained departmental support for our initiative ($50,000 for 2 years) to fund PFAC leader and administrative time, and operating costs for the group (parking, meals, and meeting supplies).
Identifying potential PFAC members was challenging and took much longer than anticipated despite multiple methods of outreach to physicians, nurses and social workers. The most successful recruitment strategies were direct visits to hospitalized patients and mailed letters from attending physicians to recently discharged patients. In total, we identified 28 potential PFAC members for screening. The screening process – in-person or telephone interviews – was essential to identify members who were 1) not acutely unwell, 2) able to travel, 3) no longer actively grieving or angry about a negative hospital experience, and 4) able to effectively communicate feedback. The main reasons potential members declined to participate were ongoing illness, limited availability, and recent bereavement.
Our first PFAC meeting occurred September 2018 with 11 members, and focused on creating a mission statement, defining operating “ground rules,” and promoting cohesion between members and leaders through team-building exercises. We have focused subsequent meetings on integrating the PFAC into our Hospital Medicine group, both by ensuring dialogue with senior leaders and by soliciting presentations from hospitalists on clinical, quality improvement, and research projects thought to benefit from direct patient and caregiver feedback.
Conclusions: Given creating a Hospital Medicine specific PFAC presents unique challenges, those looking to replicate this process should possess knowledge of patient engagement best practices and prepare to address difficult barriers.