Background: Many U.S. emergency departments (EDs) and hospitals experience critical overcrowding and capacity challenges which has been exacerbated by the COVID-19 pandemic.(1) ED boarding has been associated with a range of adverse outcomes, and pre-pandemic data suggests that racial minority patients may be disproportionately impacted.(2-4) We aim to identify the effects of patient race and boarding time on both racial discrimination and patient experience while admitted to general medicine services.
Methods: We conducted random-sample surveys of patients admitted to internal medicine services, with equal weights of Black, Indigenous people of color (BIPOC) and/or LatinX patients and non-Hispanic white patients at a large urban academic hospital from June 2023-November 2023. Boarding time was calculated as a ordinal variable to measure time-dependent effects. Our main outcomes were perceived discrimination, via the 7-item Discrimination in Medical Settings Scale, and patient satisfaction, via the 15-item Picker Patient Satisfaction scale.(5, 6) Logistic regression was used to determine the associations between boarding time and perceived discrimination and patient satisfaction, controlling for individuals’ age and sex.
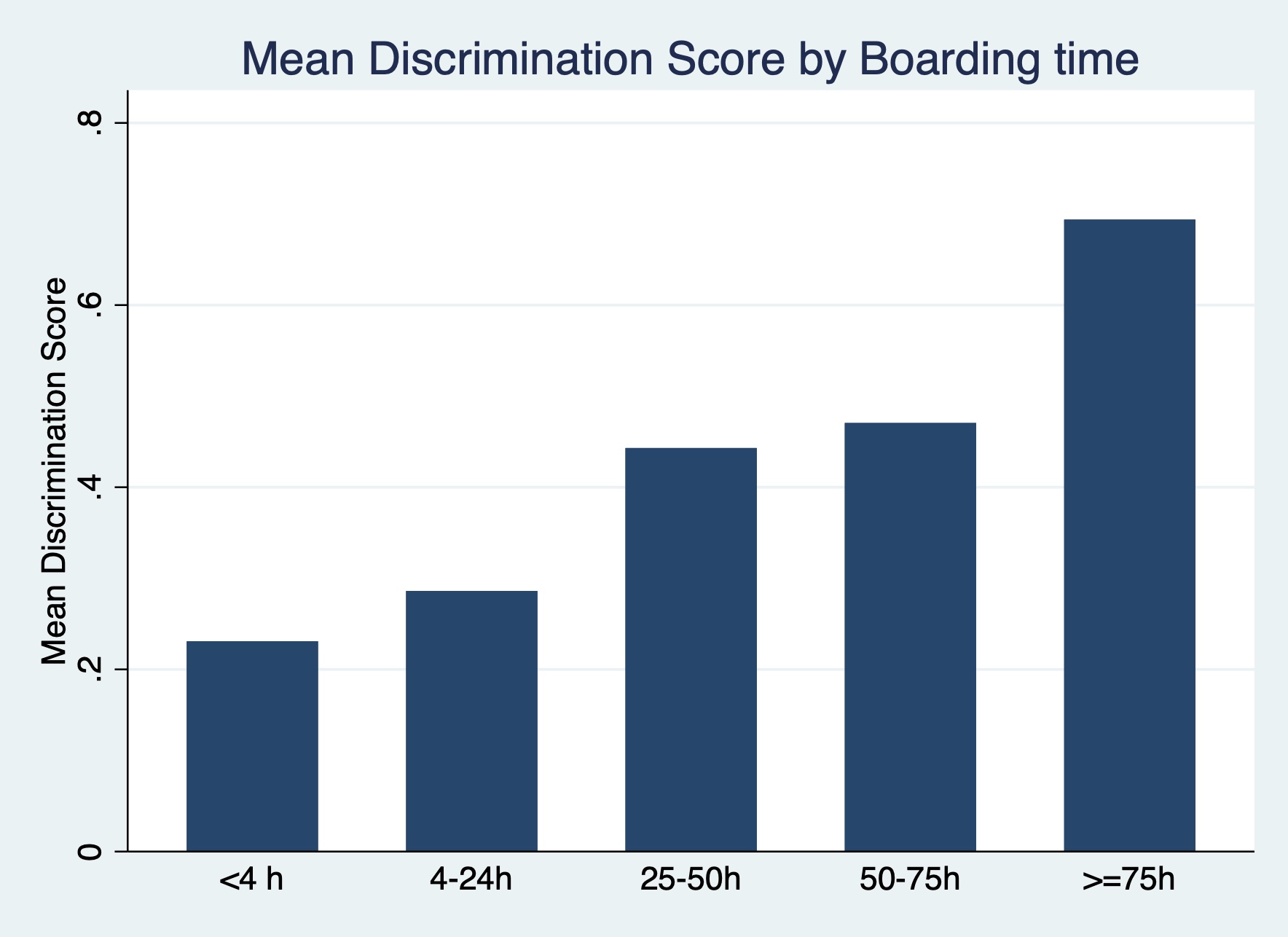
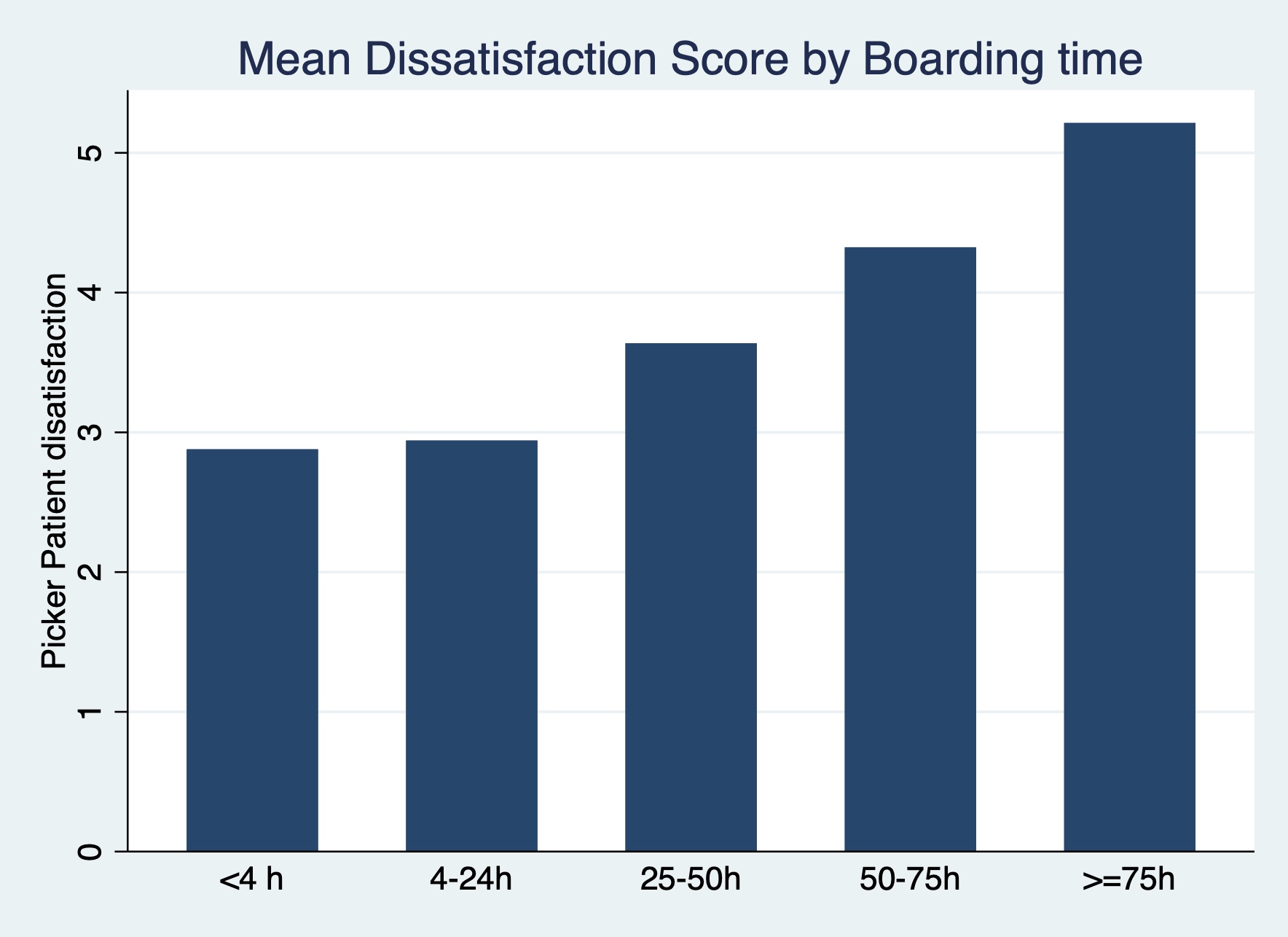
Results: Out of 370 participants, the mean age (SD) was 61.0 (17.9), 56% were women, and 42% identified as BIPOC and/or LatinX. Median boarding time was 14.4 hours. Most patients were dissatisfied with some element of their care, however this was significantly higher amongst BIPOC and/or LatinX patients (84.7% vs 73.7%, p=0.02). In comparison to white patients, BIPOC and/or LatinX patients experienced significantly more discrimination (30.6% vs 19.2%, p=0.02). Adjusting for age and sex, longer boarding times were associated with a 1.37 higher odds (95% CI 1.09-1.72) of experiencing racial discrimination, and 1.82 higher odds (95% CI 1.26-2.62) amongst BIPOC and/or LatinX patients. Boarding time was also associated with a 1.39 higher adjusted odds (95% CI 1.06-1.83) of patient dissatisfaction, with a similar trend amongst BIPOC/LatinX patients (aOR 1.62, 95% CI 0.93-2.81, p=.09).
Conclusions: Our findings suggest that longer boarding times increase racial discrimination and lower patient satisfaction for patients admitted to general medicine services, particularly for BIPOC and LatinX patients. Priority should be given to efforts that decrease emergency department boarding time for patients admitted to hospital services to improve patient quality of care and racial equity outcomes.