Background: The 2016 and 2023 AABB international red blood cell (RBC) transfusion guidelines recommend, in addition to restrictive transfusion practices, that clinicians also consider the patient’s overall clinical context when making transfusion decisions (1). However, there is little empiric data on which specific clinical factors, other than Hb, should inform transfusion decisions in hospitalized patients with anemia. Knowing which clinical factors hospitalists consider significant when making these decisions is important for determining whether variation in transfusion practice, particularly transfusion outside restrictive practices, is clinically indicated. Therefore, the purpose of this study was to identify specific clinical factors hospitalists prioritize when considering RBC transfusion and gauge their understanding of how these factors fit within current clinical transfusion guidelines.
Methods: This study was a cross-sectional survey of hospitalists at the University of Chicago. Any provider able to order RBC transfusion (attending physicians, fellows, and advanced practice providers) was eligible. Non-clinicians (Ph.D.’s) were excluded. A survey to capture which clinical factors influence transfusion decisions was designed based on a comprehensive literature review, clinical experience of the study team, and clinician focus groups. The ranked survey choices for each clinical factor included “very important”, “somewhat important”, or “not important”. Data collection occurred in June and July 2023. Descriptive statistics were used to characterize the participants, the ranking of factors clinicians considered when ordering RBC transfusion, overall provider preferences for RBC transfusion, and the understanding of risks associated with RBC transfusion.
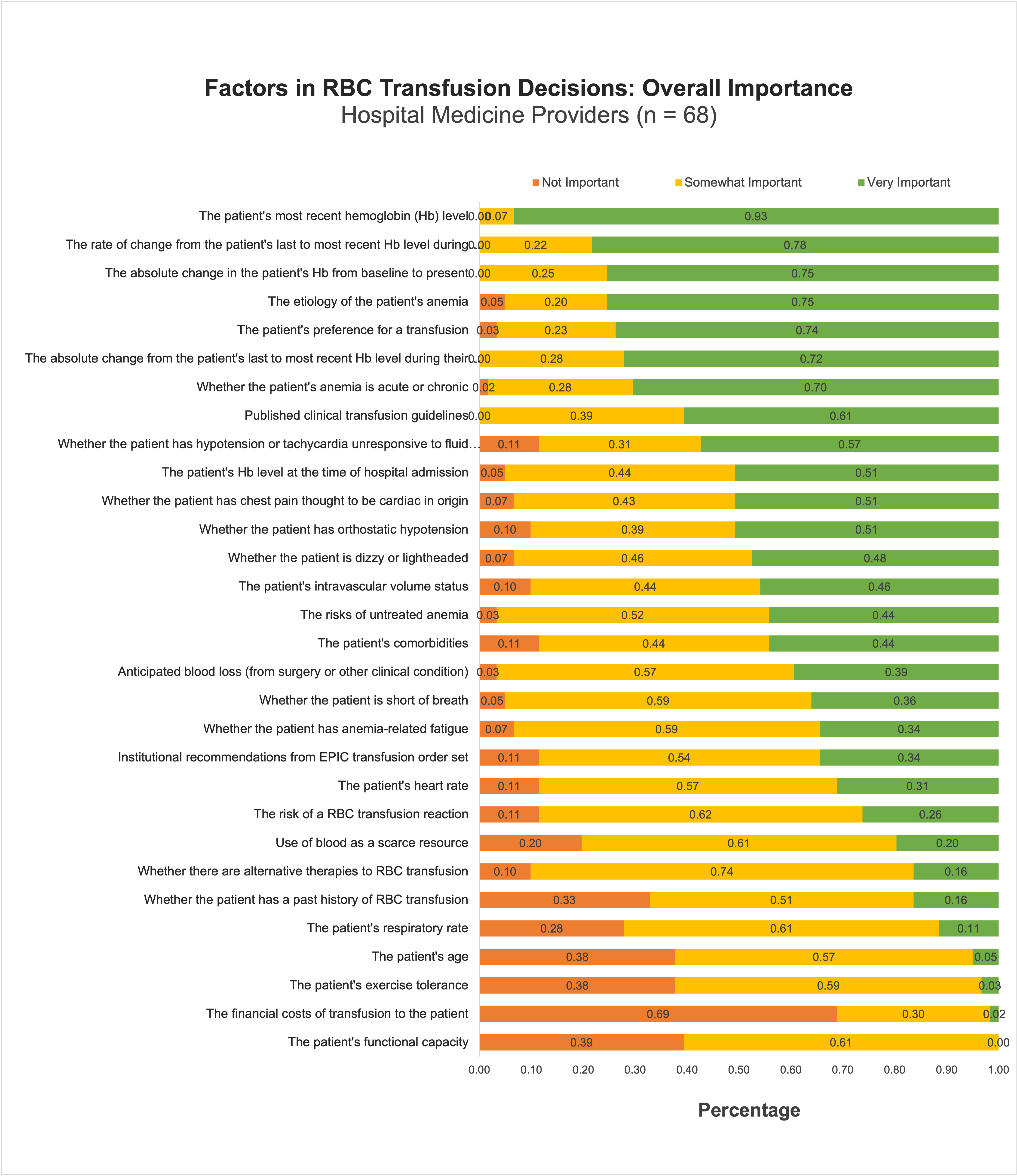
Results: A total of 68 clinicians were identified for inclusion in the study. Of these, 63 (90%) completed the survey. The mean provider age was 38 years old, 28 (46%) were female, 22 (36%) were Asian, and 31 (51%) were White.The ranking of 30 factors is reported in Figure 1. Of the top ten most important factors, five were related to Hb. Clinical factors that were seen as relatively not important included: financial costs of transfusion to the patient, patient’s functional capacity, patient’s exercise tolerance, patient’s age, and whether the patient has a history of RBC transfusion. Additionally, 84% of providers believed that anemia is a condition with significant adverse consequences and 68% believed that restrictive transfusion practice was optimal for all stable hospitalized patients.
Conclusions: Despite guidelines suggesting the significance of other clinical factors, Hospitalists still rate Hb-related factors as the most important in their transfusion decisions. Furthermore, there is wide variation in how important hospitalists believe these other clinical factors are in making transfusion decisions. Future empiric work should capture how clinical factors other than Hb impact patient outcomes.