Background: Venous thromboembolism (VTE) is a leading cause of preventable in-hospital mortality and a primary focus of quality improvement/patient safety efforts. VTE prophylaxis reduces the incidence of in-hospital VTE, but nonadministration rates—primarily attributed to patient refusal—often reach 10-15%. Notably, nonadministration of VTE prophylaxis may correlate with higher incidence of hospital acquired VTE. Prior studies showed that delivering focused educational packages to patients decreased prophylaxis refusal rates. However, this approach required a full-time health educator, a significant expense. Additionally, patients may favor receiving education directly from their physician. At MedStar Georgetown University Hospital, Medicine providers have adopted Microsoft Teams, a ubiquitous e-messaging software, for text based clinical communication. Our study assessed whether a centralized notification of VTE prophylaxis refusal to the primary provider via Microsoft Teams would decrease prophylaxis nonadministration rates on general medical wards.
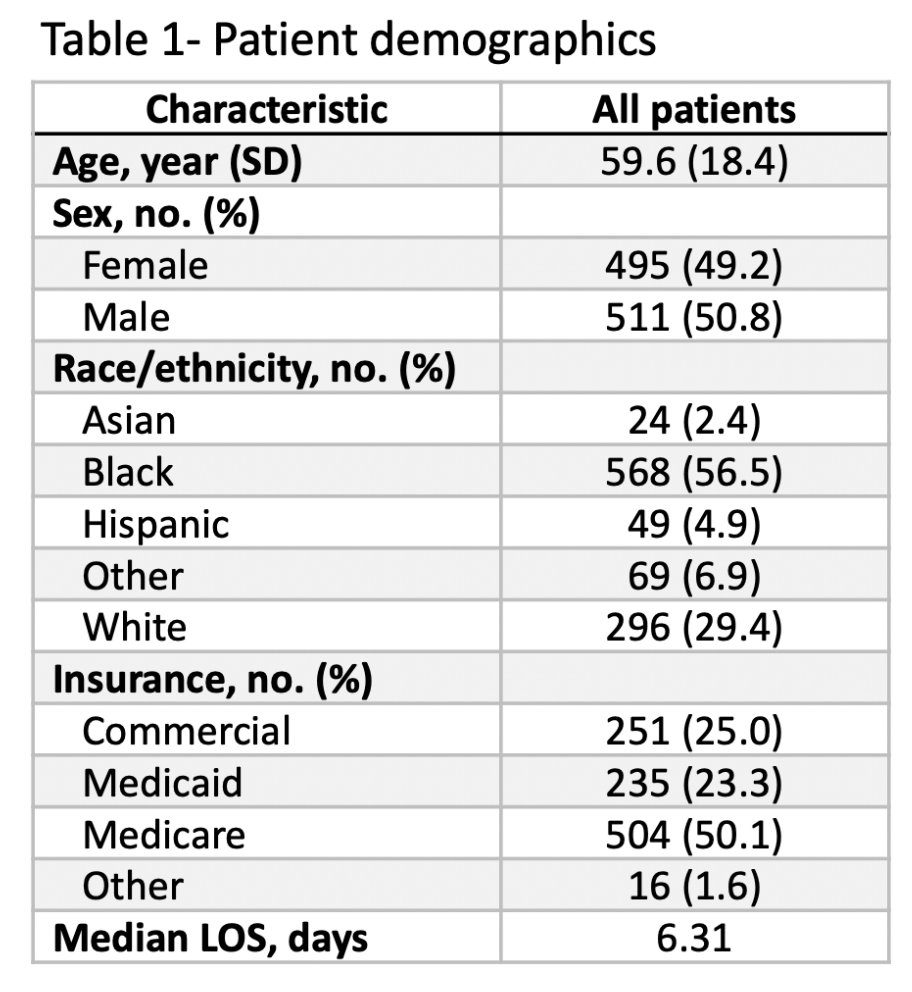
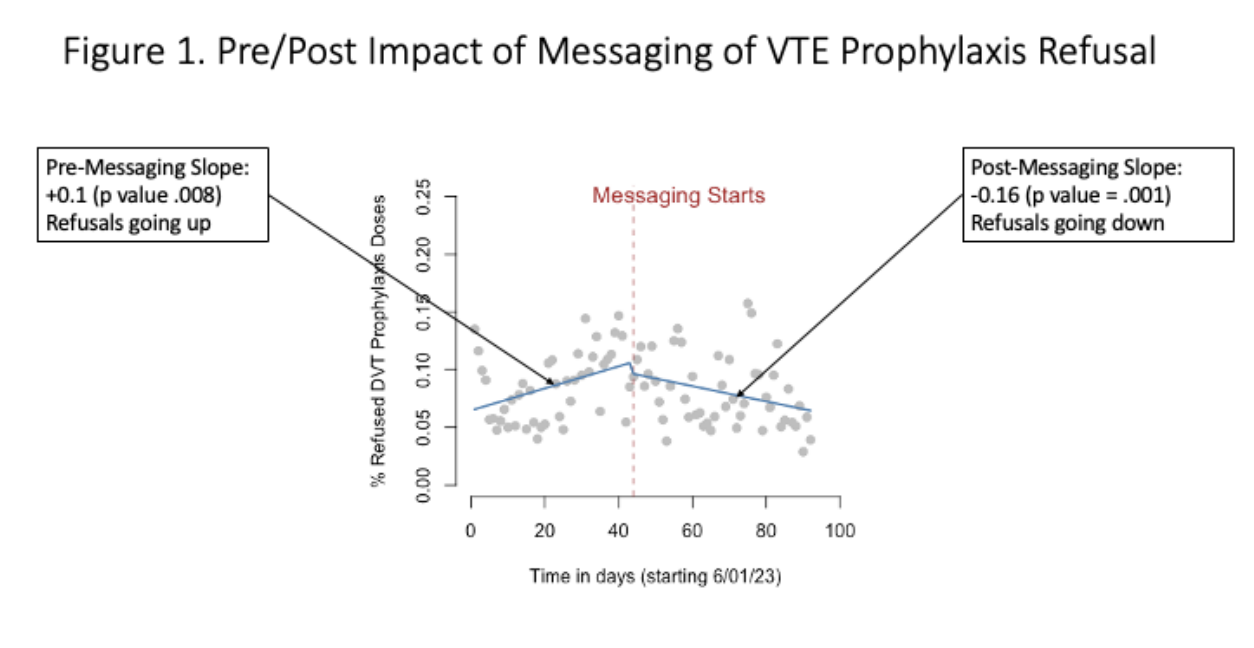
Methods: We carried out a prospective, pre/post-intervention assessment of a quality improvement project intended to decrease VTE prophylaxis refusal rates on primary medicine inpatients at an urban tertiary care center. All adult patients admitted to inpatient or observation status as medicine primary patients and prescribed pharmacologic VTE prophylaxis (either heparin or enoxaparin ordered at VTE prophylaxis dosing) were eligible. We assessed daily VTE refusal rates for six weeks before the intervention and 6 weeks after the intervention. The intervention consisted of messaging via Microsoft Teams app at a target time of either 7:00am or 1:00pm on Monday through Friday. Patient refusals were identified via an automated query of the electronic Medication Administration Record (eMAR) for any administration event documented as “refused” by nursing in the preceding 24 hours. All data was obtained via SQL query of the MedStar Analytics Platform, the data warehouse underlying the hospital EMR. An interrupted time series analysis was carried out with an apriori outcome of daily change in VTE refusal rate using R statistical program.
Results: A total of 1006 eligible patient admissions were identified spanning the 6-week baseline and 6- week intervention periods (see Table 1). The average daily refusal rate pre-intervention was 6.5% with a positive daily change of +0.1% (p = 0.008), consistent with a trend of rising daily VTE prophylaxis refusal rates prior to the intervention. Post-intervention, the daily change rate became negative at -0.16% (p=0.001) consistent with a declining trend in VTE prophylaxis refusal rates.
Conclusions: Implementation of centralized, systematic text messaging to providers of VTE prophylaxis patient refusals was associated with a decreasing daily refusal rate in the post-intervention period in contrast to a rising rate of refusals prior to the intervention. This is the first study to show a positive impact of direct provider messaging on minimizing VTE prophylaxis nonadministration rates. Compared to proven methods of lowering VTE refusal rates including the use of full-time health educators, direct messaging to providers may be a lower cost intervention which leverages the strength inherent in the provider-patient relationship.