Background: Social determinants of health (SDOH) are thought to account for up to half of modifiable outcomes related to health. Children from minority groups and/or lower socioeconomic backgrounds are at higher risk for hospitalization. Efforts have been made to screen for social risk factors in the outpatient setting. However, few studies describe inpatient SDOH screening even though hospitalization may be when a family’s social needs become especially evident. In 2022, our institution implemented nurse-driven screening for food, housing, and transportation insecurities for all inpatient pediatric patients. However, patients who screened at risk did not consistently receive resource referrals. Our Quality Improvement initiative sought to: 1) improve the rate of completed social work consults and 211-resource referrals in hospitalized pediatric patients who screened at risk for insecurities in the SDOH domains of food, housing, and transportation and 2) improve the rate of screening of SDOH.
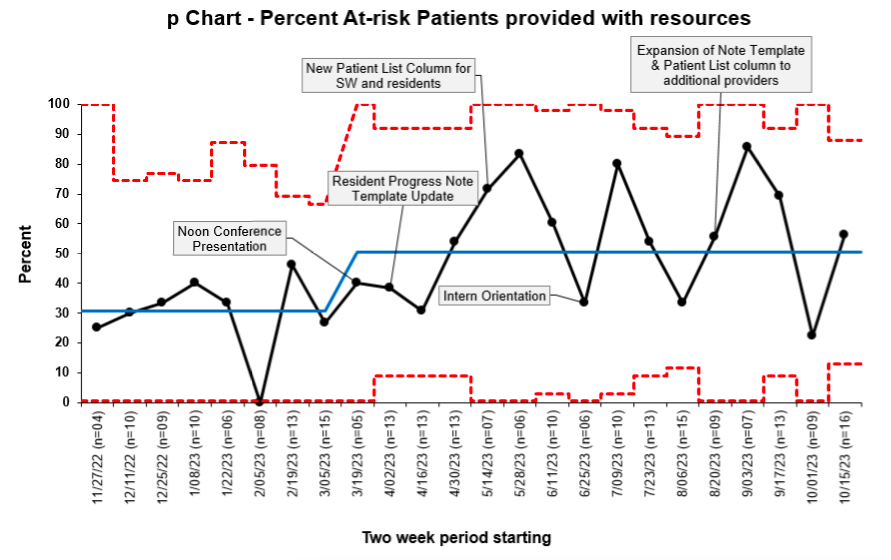
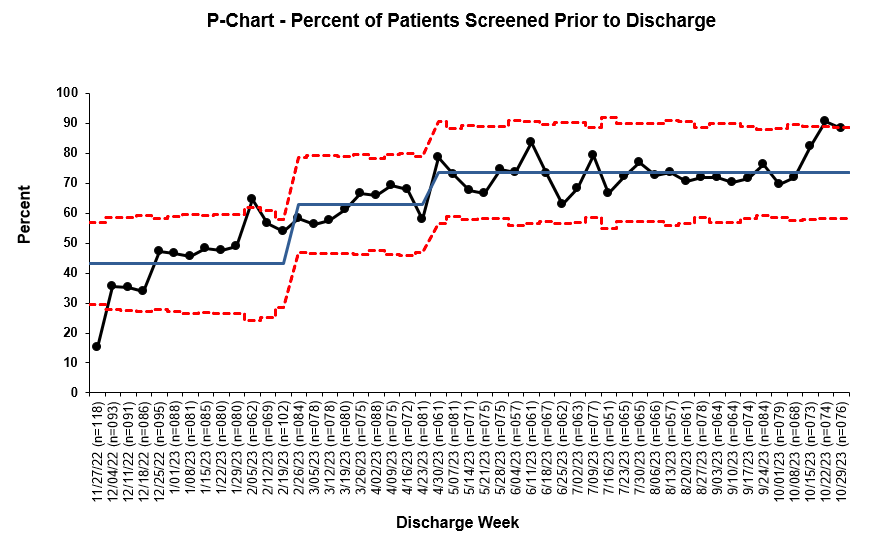
Methods: Using the Model for Improvement framework, we began by developing a key driver diagram and workflow process mapping. We then iteratively enacted Plan-Do-Study-Act (PDSA) cycle interventions. These included targeted in-person education during new intern orientation, residency noon conference, and advanced practice provider group meetings, as well as email education to providers, nursing, and social work. Additionally, we provided unit-specific screening adherence reports to nurse educators on each unit and encouraged multidisciplinary engagement on care coordinator and social work rounds. Central to our project were iteratively adapted clinical decision support interventions in the electronic health record (EHR) that included a passive rule-based text in commonly used provider note templates both in the admission note and daily progress notes. We also created a patient list column for providers and social workers indicating whether the SDOH screening had been completed and if any areas of need were identified. We tracked outcome and process metrics on statistical process control charts (Figures 1 and 2). Our primary outcome metric (Figure 1) was the percentage of at-risk patients who received a completed social work consult addressing the identified risk factors, e-referral in the after-visit summary to a 211 directory community resource, or an order to our emergency food pantry. Our process metrics included the percent of patients who were screened (Figure 2) and the percent of at-risk patients who had a social work consult order.
Results: Over nine months, the mean percentage of at-risk patients who received targeted resources improved from 30.7% to 50.8%, with special cause variation observed (Figure 1). Concurrently, the mean percentage of patients screened prior to discharge improved from a baseline of 43.1% to 73.5% (Figure 2). The percentage of social work consults ordered remained at 60%.
Conclusions: Widespread adoption of social risk factors screening via the EHR for hospitalized pediatric patients allows for discrete data capture. Inpatient stays are a particularly valuable time in which to screen children. Next steps include enabling outpatient follow-up by including SDOH screening results in discharge summaries and boosting screening and follow-up through audit and feedback with additional multidisciplinary unit-based engagement.