Background: Aggressive EOL treatments in advanced cancer patients are associated with low-value care and frequently lead to unnecessary hospitalizations. Since 2012, the National Quality Forum (NQF), American Society of Clinical Oncology (ASCO), and Centers for Medicare and Medicaid Services (CMS) have adopted EOL quality measures to reduce aggressive care. Using these measures, we conducted a systematic review of the literature to explore what interventions are associated with reductions in aggressive EOL care in cancer patients.
Methods: We searched MEDLINE via Ovid, Cochrane, CINAHL, EMBASE, Scopus, and PsychINFO. We developed a comprehensive search strategy using the following concepts: EOL care, aggressive or intense care, and cancer. We included randomized control trials (RCTs), quasi-experiments, and observational studies. Studies that did not have a clear intervention or exposure variable and/or did not explicitly aim to reduce aggressive EOL care or improve quality of EOL care were excluded. We developed a taxonomy to organize our findings using the Systems Engineering Initiative for Patient Safety (SEIPS) model derived from human factors engineering. The study protocol was registered with the PROSPERO register of systematic reviews (CRD42018087528).
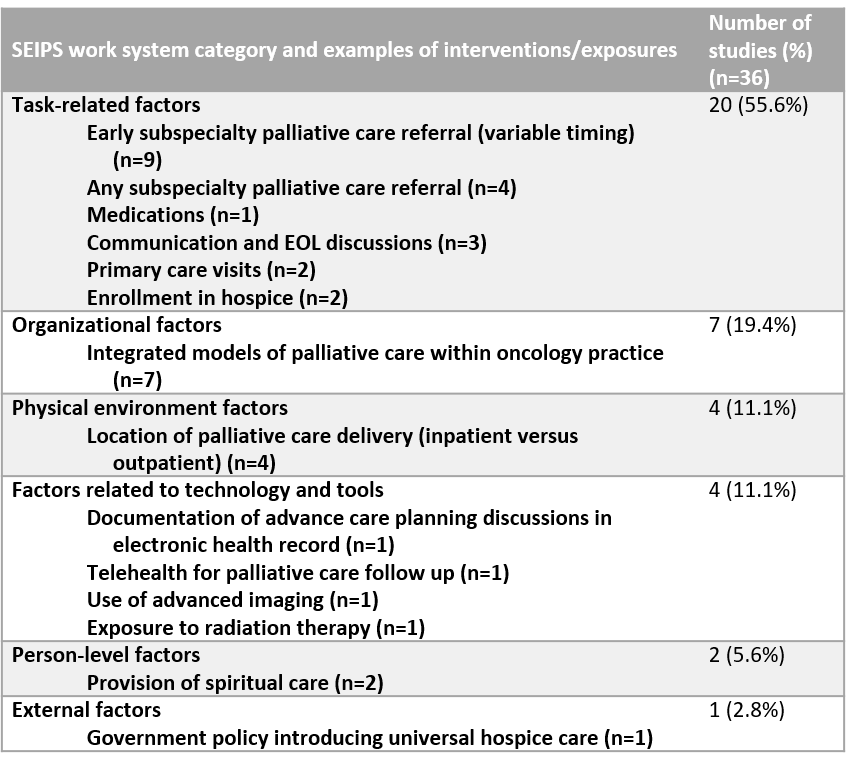
Results: Of the 3,881 studies identified by our search, 271 were included based on title and abstract review, and 36 met the final inclusion criteria after full-text review. Five studies were RCTs. Thirty-two studies used validated or nationally endorsed measures of aggressive EOL care, while 26 used additional unendorsed or un-validated measures. Only 8 studies linked quality measures with patient- or caregiver-reported outcomes. Based on our taxonomy of SEIPS work system categories, we found that interventions targeting task-related factors were most common (n=20), whereas the least prevalent targeted external factors (n=1). The prevalence and types of interventions are summarized by SEIPS category in Table 1. Meta-analysis was not performed due to heterogeneity of interventions and outcome measures. Interventions were highly variable in their ability to significantly improve measures of aggressive care at EOL in cancer patients.
Conclusions: Quality measures to reduce overly aggressive EOL cancer care, including hospitalizations, are used inconsistently by investigators. Interventions to improve aggressive EOL care have had mixed success. More studies are needed to assess the efficacy of interventions to reduce aggressive EOL cancer care, particularly those that link quality measures with patient- and caregiver-reported outcomes.