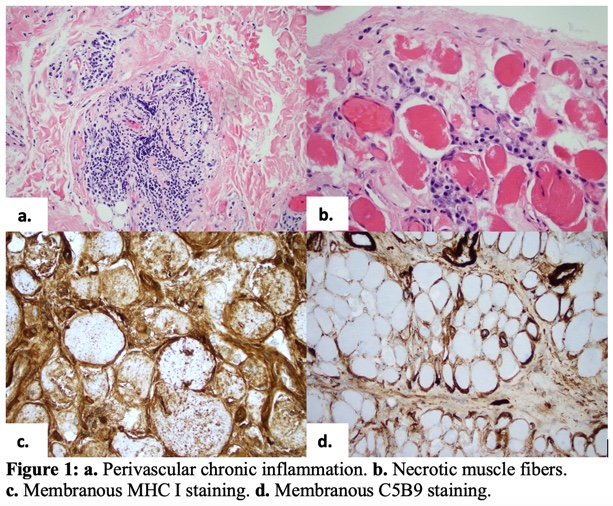
Case Presentation: An 80-year-old man presented to the hospital with recurrent falls and generalized weakness over six months. Past medical history was notable for dementia, hypertension, and peripheral polyneuropathy. This was his fifth admission for weakness and falls with elevated CPK concerning for rhabdomyolysis, previously treated with intravenous fluids, physical and occupational therapy, and discharged back to his memory care facility. On this admission, the patient was found down for two hours at his nursing facility. He reported significant proximal muscle weakness in both the upper and lower extremities with inability to reach his arms above his head or feed himself.Physical exam demonstrated roughness and fissuring of the distal phalanges bilaterally and decreased sensation with 3/5 strength in the deltoids and hip flexors. Laboratory studies were significant for CPK 17,085, ESR 70, CRP 2.6, Aldolase 56.1 (1.2-7.6). Myositis panel was positive for OJ (ISOLEUCYL-TRNA SYNTHETASE) antibodies. CT of the thoracic spine for skeletal surveillance showed scarring and peripheral fibrotic lung changes. Muscle biopsy was obtained and consistent with active necrotizing inflammatory myopathy [Figure 1]. The patient received 40 mg of prednisone daily with noticeable and rapid improvement in proximal muscle weakness within the next 48 hours. This was consistent with anti-synthetase syndrome, a sub-class of idiopathic inflammatory myopathies.
Discussion: Rhabdomyolysis is common after prolonged falls and is associated with elevated CPK. The degree of CPK elevation often correlates with the risk of renal injury and should rapidly normalize with fluid resuscitation. In this patient, after fluid resuscitation, levels decreased but remained elevated around 4-6k, prompting further investigation with muscle biopsy. The degree of CPK elevation in dermatomyositis (DM) and polymyositis (PM) varies greatly and can be up to 100 times the upper limit of normal. Patients with anti-synthetase syndrome often have an autoantibody in the anti-tRNA synthetase group (Jo-1, PL-7, PL-12, OJ, EJ, Zo, Ha, and KS), with anti Jo-1 being the most common [1]. Autoantibodies directed against aminoacyl-tRNA synthetases are found in approximately 25% to 35% of patients with PM and DM and of those anti-OJ antibodies were found in less than 2% [2].Distinctive systemic manifestations that help to distinguish anti-synthetase syndrome from DM/PM include interstitial lung disease, hyperkeratosis of the dorsal hands and fingers referred to as “mechanic’s hands,” arthralgias, and Raynaud’s phenomenon. All three of these findings were present in this patient but are commonly overlooked due to high prevalence in the elderly population. Diagnosis with muscle biopsy and serum studies for autoantibodies is important to direct therapy and duration of treatment. Case reports have shown that interstitial lung disease patients with anti-OJ autoantibodies have better prognosis and good responses to glucocorticoid monotherapy [3].
Conclusions: Falls are common reasons for admission in elderly patients with dementia. It is important that hospitalists consider other etiologies of weakness and fragility in these patients who present with recurrent falls and evidence of rhabdomyolysis. Patients presenting with elevated CPK that does not normalize after fluid resuscitation should undergo further testing. Myositis can be easily overlooked in this patient population, and treatment can offer symptomatic relief and improved quality of life.