Background: The American Board of Internal Medicine and the Society of Hospital Medicine have identified routine laboratory testing of stable inpatients as one source of low-value care.1,2 As it is estimated that upwards of 21% of all lab tests represent inappropriate overutilization,3 reducing unnecessary testing could have a significant impact on cost saving, limiting waste, and improving healthcare quality. Beyond minimizing iatrogenic anemia and reducing costs,4,5 another benefit of reducing superfluous lab testing is decreasing healthcare’s carbon footprint. If the US healthcare system was its own nation, it would be the 13th largest emitter of greenhouse gas emissions. Each basic metabolic panel produces 99 grams of CO2,6 and given the volume of inappropriate tests performed annually, reducing unnecessary lab testing at scale could have a meaningful impact on the carbon footprint of US healthcare. We designed a multifaceted behavioral and educational intervention integrating the concepts of sustainability and high-value care to decrease the total number of basic lab tests ordered for clinically stable inpatients and to assess the attitudes and ordering practices of medical residents.
Methods: We conducted a six-month prospective cohort pilot on two general medicine resident teams at a single tertiary hospital. One team served as control, while the other 1) viewed an educational video on the effects of unnecessary lab testing with a focus on the adverse environmental impacts of US healthcare, 2) implemented daily team-based reviews of basic lab orders, and 3) received thrice weekly emails about said lab reviews. Basic lab tests included the Basic Metabolic Panel, Complete Blood Count, Magnesium, Phosphorus, Liver Function Tests, and PT-INR. Intervention team residents received pre-and post-surveys to assess attitudes and ordering behaviors. We performed a series of statistical tests including t-test, propensity score, and non-inferiority analyses to assess differences in the total number of basic lab tests per patient per day and total venipunctures per patient per day. Secondary outcomes included patient length of stay (LOS), inpatient mortality, ICU transfers, and 30-day readmission and mortality rates.
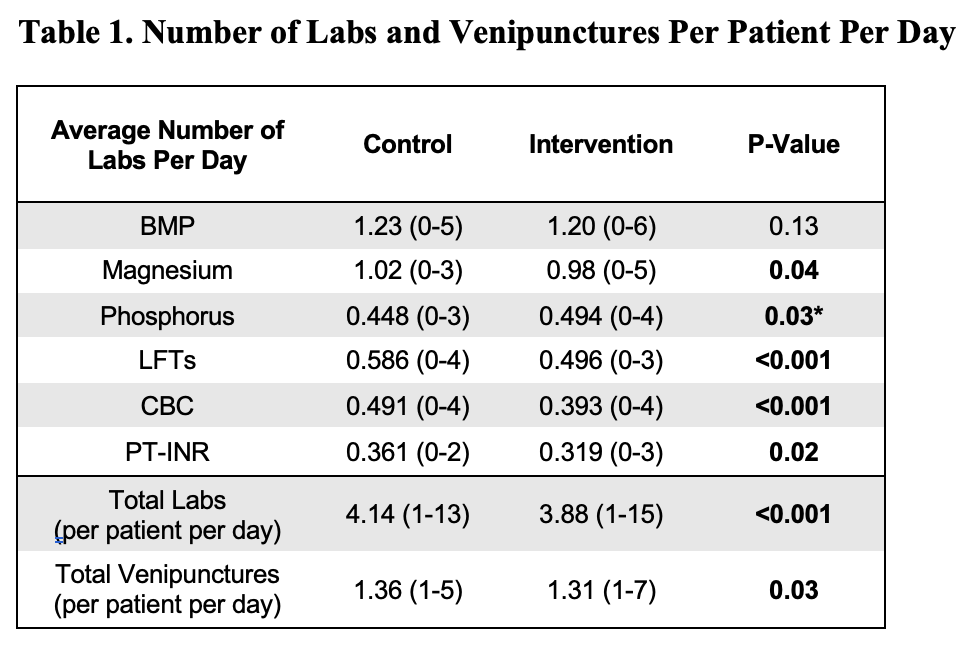
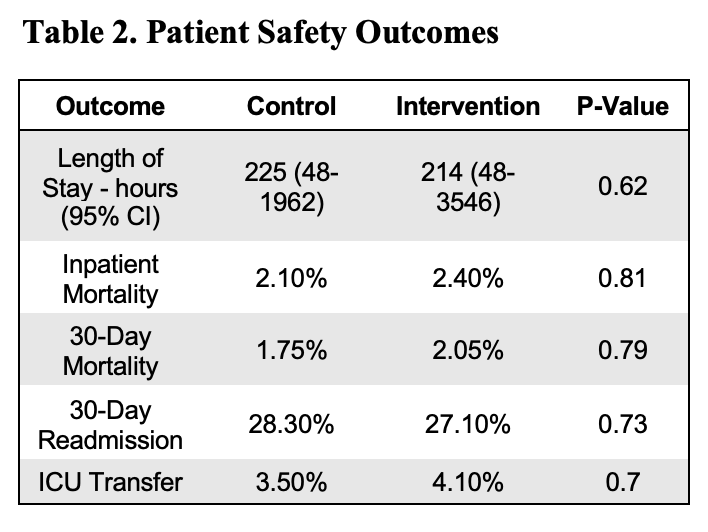
Results: The provider cohort consisted of 72 residents and 48 attending physicians evenly split between the intervention and control teams, caring for 287 and 293 patients, respectively. Baseline patient demographics were similar between groups. Patients treated by the intervention team had statistically significant decreases in total labs and venipunctures per patient per day compared to patients treated by the control team (Table 1) without significant differences in LOS, inpatient mortality, ICU transfers, and 30-day readmission and mortality rates (Table 2). Survey data suggested that the intervention promoted psychological safety around de-escalating lab orders and that residents more frequently assessed and de-escalated basic lab orders.
Conclusions: This pilot of an educational and behavioral intervention integrating concepts of environmental sustainability and high-value care meaningfully impacted resident ordering behavior, leading to significantly fewer lab tests and venipunctures without compromising key patient safety outcomes. Survey results also shed light on factors motivating serial lab testing that can be targets for future interventions.