Background: Understanding a hospitalist’s efficiency is important to identify opportunities to provide support and prevent burnout (1). This is key when onboarding new hospitalists, as early intervention can lead to rapid improvement and a long-term sustainable career. The evaluation of hospitalist efficiency can be difficult and is often thought to require close clinical shadowing or patient-level encounter review metrics, such as length of stay or cost of care. Outpatient providers use “pajama time” or time spent in the electronic health record (EHR) at night, to evaluate efficiency, but hospitalists are not afforded the opportunity to take work home (2). However, note completion time is a metric that is relatively easy for hospitalist leaders to obtain from the EHR and can clearly be put into context for any hospitalist group’s standard workflow. The aim of this study is to evaluate the utility of using note completion time as a simple surrogate for clinical efficiency.
Methods: The study was conducted with a single site hospitalist group based at a large, urban, academic tertiary referral center. The timeframe of the study was from July 10, 2019 until November 10, 2019, which included the start of 14 new hospitalists within the group. Notes from the EHR designated as “Progress Note” were chosen for inclusion as most likely representative of real-time work in direct care settings, as new patient History and Physical notes are often completed during off-hours shifts and Discharge Summaries are not always completed at the time of care. Coding query responses in the study institution are captured in Progress Notes, so any note with a completion time >1000 minutes was excluded from the analysis. Notes completed before 5:00pm, which is the set time of sign out for the group’s workflow, were designated as “On-Time” and considered a marker of efficiency. A balancing measure of efficiency was duration of note completion. Notes taking <3 minutes to complete were flagged as “Short” in the analysis, potentially representing only copy-forward. Proportions of On-Time and Short notes were calculated during the first 2 months of work and the subsequent 3 months. The trends of both measures over time were reviewed by group leadership and shared with individual providers.
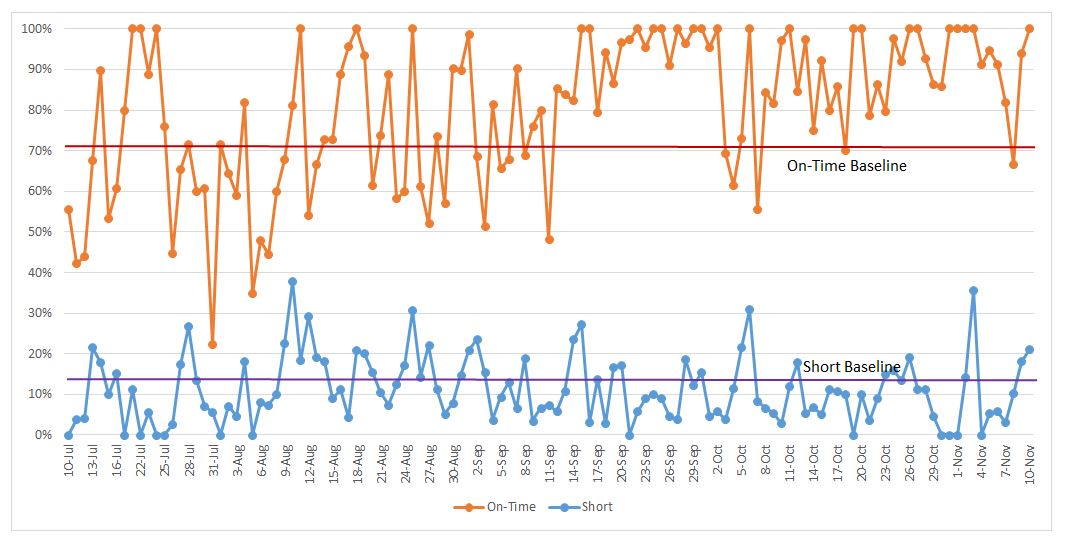
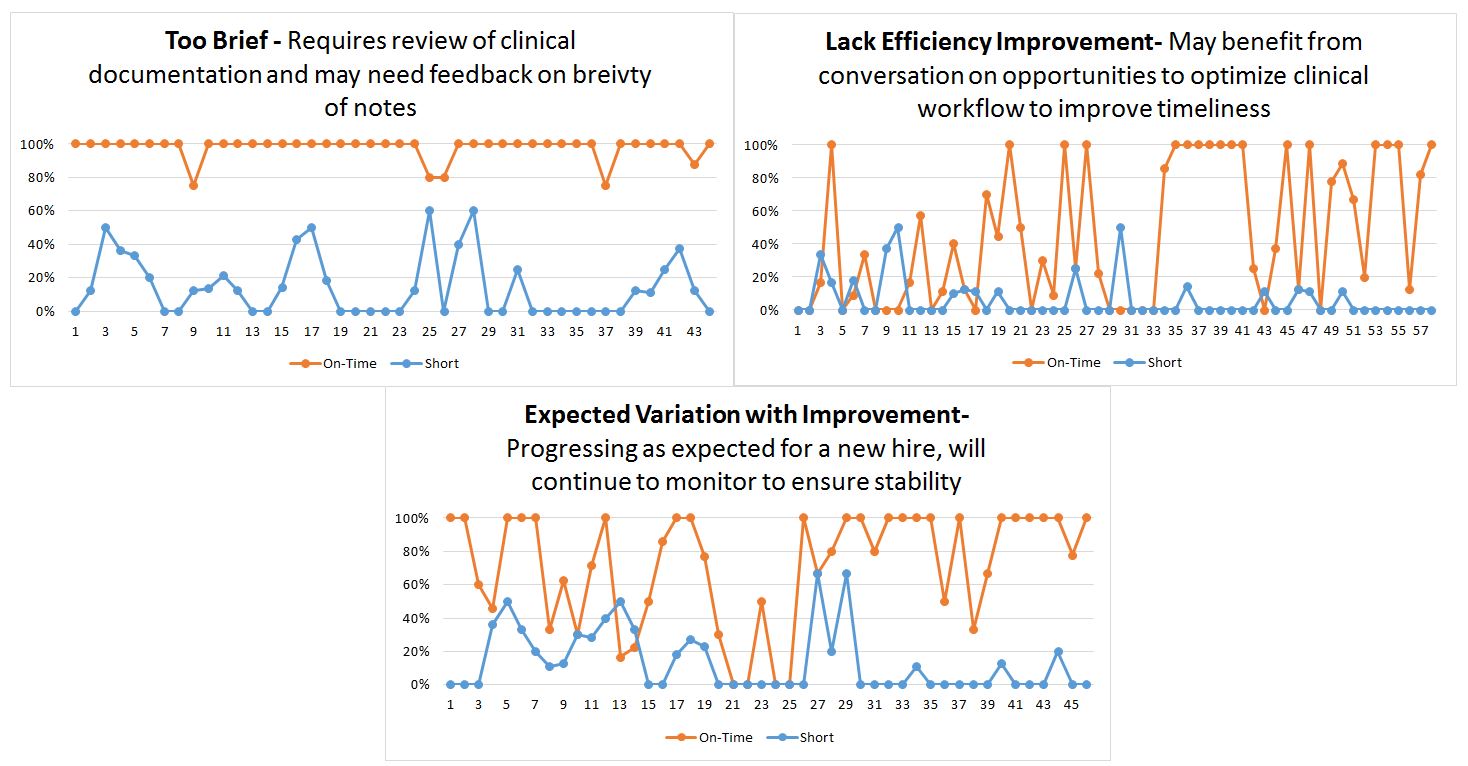
Results: A total of 3730 notes were included in the analysis, with a median note volume per provider of 273.5 (IQR 188-366). Overall, the proportion of On-Time notes significantly increased from 71% during the first 2 months to 89% during the latter 3 months (p<0.0001). Short notes significantly decreased in frequency between the two time periods (14% vs 11%, p=0.03). Graphically trended over time, there were only 6 days in the last 3 months with proportions of On-Time notes below the initial period’s baseline (Figure 1). At the provider level, review of trends over time revealed multiple new hospitalist phenotypes that could prompt further review and possible assistance, or offer the opportunity provide reassurances (Figure 2).
Conclusions: Timely completion of progress notes can serve as a simple marker of provider efficiency and is shown to improve over the course of time for new hire hospitalists. Review of individual provider note completion over time can help to identify those who may need further review, or additional support as an early effort in burnout prevention for new hospitalists.