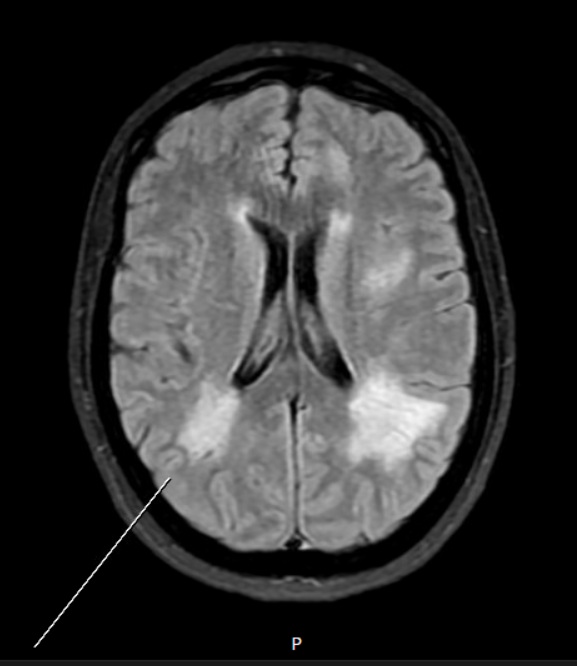
Case Presentation: A 40yo woman with no significant past medical history presented to her optometrist with three months of progressive intermittent blurry vision. She was diagnosed with bilateral papilledema and advised to urgently follow up with her primary doctor. Upon evaluation she denied any symptoms aside from her visual changes. Her heart rate was 132 and her blood pressure was 144/82; the remainder of her physical exam was normal. Outpatient workup revealed TSH 1.15, Free T4 1.9, and Total T3 > 500. MRI Head with and without contrast confirmed papilledema and noted confluent areas of T2/FLAIR elongation within the bilateral periventricular and subcortical white matter extending to the bilateral thalamic regions and cerebellar hemispheres (Figure 1). Given concern for posterior reversible encephalopathy syndrome (PRES), she was immediately sent to the emergency department, and on arrival her blood pressure was 300/192. She was admitted for aggressive antihypertensive therapy, including a brief continuous nicardipine infusion, and was transitioned to propranolol and methimazole prior to discharge. Ultimately her Thyroid Stimulating Immunoglobulin (TSI) and Thyroid Receptor Antibody (TRAB) were found to be elevated and radioactive iodine uptake scan identified diffuse iodine uptake in the bilateral thyroid lobes, diagnostic of Graves’ Disease.
Discussion: This case illustrates the uncommon clinical entity of T3 Thyrotoxicosis, in which patients experience signs and symptoms of excess circulating thyroid hormone with normal to minimally elevated Free T4. Our initial differential was broad, as we considered pituitary dysfunction (such as a pituitary adenoma causing excess secretion of TSH), thyroid dysfunction (such as Graves’ Disease causing inappropriate secretion of thyroid hormone), and end organ dysfunction (such as thyroid hormone resistance causing decreased sensitivity of end organs to circulating thyroid hormone). However in each of these cases we would expect to observe either high or low levels of TSH, rather than normal levels as seen here. We did contemplate the possibility of assay interference, as it was later realized that the patient was taking multiple over the counter supplements containing biotin. Ingestion of biotin above the recommended daily amount can cause spurious results on thyroid function testing when using the biotin-streptavidin affinity assay, such as falsely low TSH and high Free T4 and Total T3. We repeated this patient’s thyroid function tests following discontinuation of biotin for more than forty-eight hours, and they remained consistently abnormal.
Conclusions: Graves’ Disease is an autoimmune disease most common in young adult women between the ages of 20 and 50, accounting for up to eighty percent of all diagnosed cases of hyperthyroidism. Typically thyroid function tests reveal high Free T4 and Total T3, with appropriately low TSH. In some cases, there may be normal TSH and a disproportionate increase in serum T3 compared to serum T4, thought to be due to either excess conversion of T4 to T3 or excess production of T3. Guidelines currently recommend screening for suspected thyroid dysfunction with TSH, yet this case emphasizes the importance of comprehensive thyroid function testing for high clinical suspicion of thyrotoxicosis even with normal TSH. This case also suggests that treatment with propylthiouracil (which reduces peripheral conversion of T4 to T3) may be preferred over typical treatment with methimazole in certain presentations of Graves’ Disease.