Background: Hospital Medicine (HM) practices have traditionally utilized an extended ‘7 on/7 off’ (7/7) schedule. Occupational Health studies suggest that such schedules can increase physiologic and psychologic stressors (Keller). Despite their prevalence, the effects of extended scheduling on physician well-being and performance are unknown. We sought to study the effect of 7/7 scheduling on well-being and performance.
Methods: Fourteen physicians participated in a prospective cohort study over a 2 month period in the fall of 2018. Seven physicians followed a 7/7 schedule and 7 physicians followed a schedule with 4-5 days working followed by 4-5 days off (4/5). A telephone survey evaluating fatigue (mental exhaustion, personal time), professional satisfaction (work enjoyment, perception of care quality), and workload (daily census) was administered to participants on the first, middle, and last days of a block. For each cohort, the first working day was compared to the middle and last days. An ⍺-level of 0.05 was significant. For operational purposes, we considered an ⍺-level of 0.2 to indicate an actionable trend.
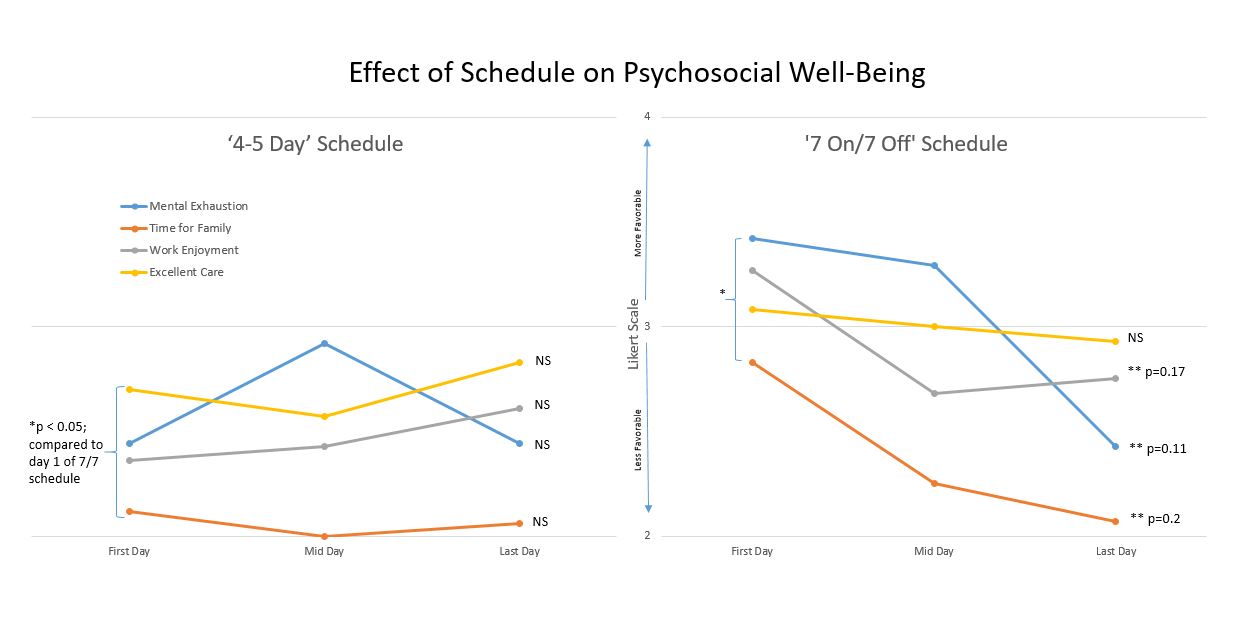
Results: The survey response rate was 66% (110/167). On the first day of service, a statistical difference favoring the 7/7 cohort was found in the mental well-being, time for family, and work enjoyment domains. Within each pilot group, comparisons of well-being on the first and last days did not achieve statistical significance in any domain. However, by the seventh day of working for the 7/7 cohort, trends towards increased mental exhaustion (p=0.11), decreased family time (p=0.2), and decreased work enjoyment (p=0.17) were observed (Figure). There was no difference in workload between the two cohorts. 86% (6/7) of the 4/5 participants recommended continuation of the 4/5 scheduling option.
Conclusions: Our pilot study suggests that a 4/5 work schedule has an unfavorable impact on well-being on the first day of service. Whether this difference is attributable to schedule properties or confounders intrinsic to the cohort participants is uncertain. Further, we found that physician well-being may be adversely impacted by the seventh day of a 7/7 schedule and these effects were mitigated by 5/4 schedules.
We intend to expand the pilot to improve our ability to detect differences in perceptions of performance and well-being. We also plan to compare objective measures of performance (length of stay, readmission, patient satisfaction) and well-being (cross-over survey results, retention rate, physician engagement) over time.
A large majority of the 5/4 cohort felt it should be incorporated into our practice. Alternative scheduling models may provide a simple, cost-neutral method to improve physician wellness and reduce HM physician burnout.