Background: Physician burnout has been alarmingly high with over 50% of practicing physicians in the U.S. reporting burnout. Of which, general internal medicine displays some of the highest rates. A recent study was published in December 2021 examining the topic of burnout from the perspective of academic hospitalists at Froedtert Hospital and the Medical College of Wisconsin (MCW). The results of this cohort found a higher level of physician burnout than average (62%), with common agreement about factors leading to burnout as well as the consequences of burnout. The current project seeks to expand upon the results of this previous study by assessing wellness strategies and institutional recommendations to mitigate burnout.
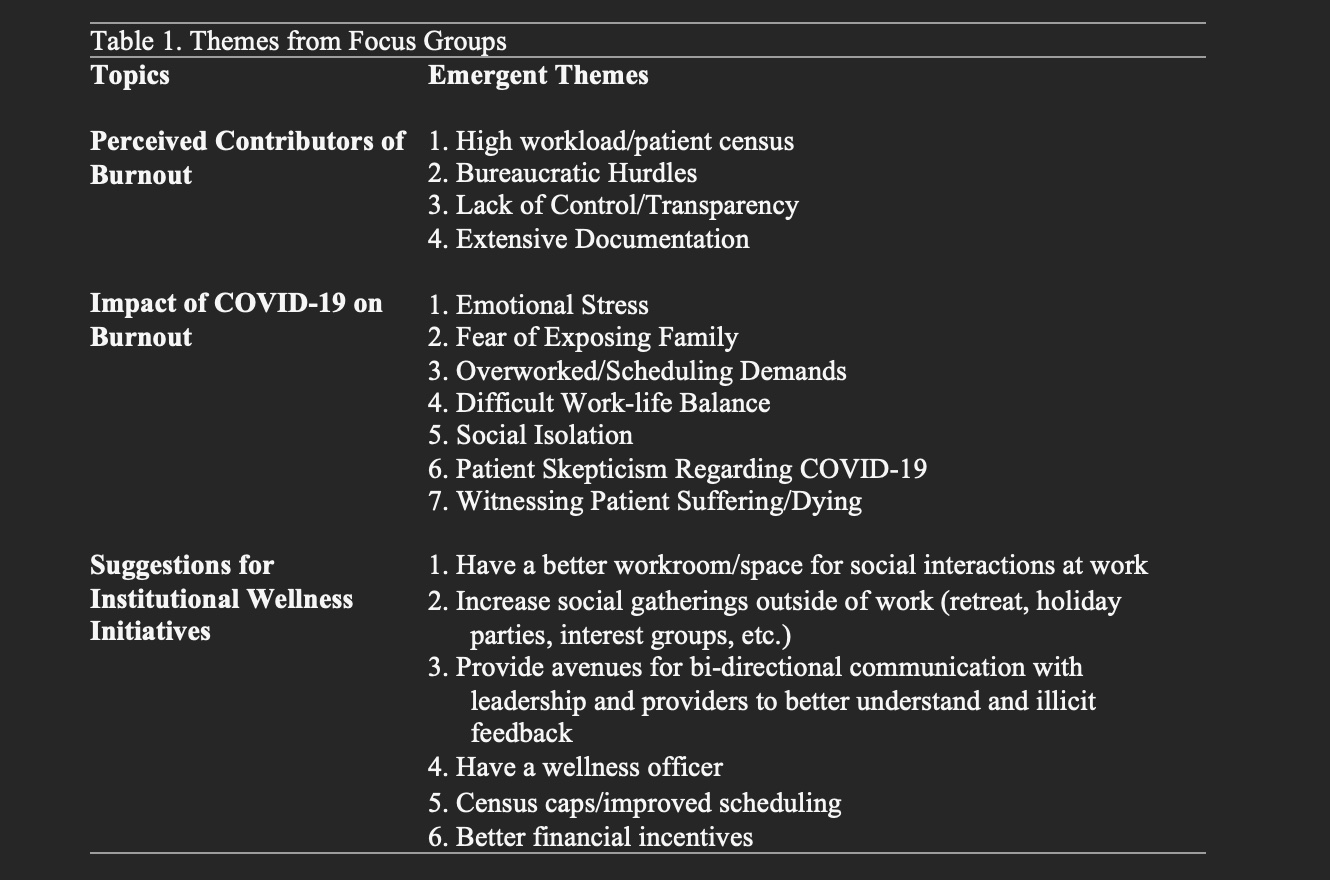
Methods: Nineteen academic hospitalists at Froedtert Hospital were recruited to participate in a series of qualitative, semi-structured interviews and focus groups. Froedtert Hospital is a 702-bed academic medical center and the primary adult teaching affiliate of the Medical College of Wisconsin (MCW). An invitation letter with details about the study was emailed to the entire hospitalist group. The letter highlighted the importance of the current study and emphasized voluntary participation. The questions focused on contributors to burnout, the impact of COVID-19, and strategies to improve wellness and reduce burnout. The focus groups were audio-recorded, transcribed, and coded for emergent themes using Taguette, an open-source qualitative data analysis software.
Results: The most common suggestion was increasing social interactions to allow providers to share experiences, seek guidance from one another, and foster a sense of community overall. This included a better workroom as well as increasing social gatherings outside of work. There was a desire for a workroom with windows, increased space, snacks, coffee, and comfortable seating. It was also noted that space constraints have led to new hires being scattered, further increasing isolation. Suggestions for social interactions outside of work included a retreat, arranging activity groups for like-minded individuals, and holiday parties. Another suggestion stressed throughout the focus groups was providing avenues for two-way communication between leadership and providers to share concerns and illicit feedback, allowing providers to feel more empowered. Additionally, physicians desired streamlining clinical work, noting that small tasks or “asks” by management are burdensome and do not improve quality of care.
Conclusions: Social isolation and lack of effective communication between providers and leadership contributes to fatigue, frustration, and may worsen burnout. This can be mitigated by enhancing community and fostering collaboration in decision making which may alleviate stress and reduce burnout. A crucial first step to combat burnout is to encourage a work environment that values clinician well-being and proactively works to increase job satisfaction.